In China the rapid development of the COVID-19 outbreak and subsequent restrictive quarantine measures (e.g., home isolation) had a profound psychological impact on most people (Hu et al., 2022). During this period, new military recruits faced not only the requirement of adjusting to the military environment for the first time but also pressure related to the coronavirus and reduction in the work income of family members, along with the social alienation that occurred as a result of distancing and isolation measures (Wynn et al., 2020). Military training exposes new recruits to a variety of stressors, such as intensive physical training, stringent management, military discipline, and compressed free time (Clemons, 1996). According to recent studies of military personnel, stressful situations are frequently accompanied by high levels of anxiety (Lucier‐Greer et al., 2022; Yakobi et al., 2022). Individuals whose anxiety reaches a level at which their functioning capacity is reduced have a higher risk of developing cognitive impairment (Clemons, 1996; Markovitz, 1993) or depression (Surtees & Wainwright, 1996), and of committing suicide (Conner et al., 2012). Military culture emphasizes obedience and operational unity, which can cause stress and makes individuals more likely to exhibit aggression, and which can affect troops’ morale and combat effectiveness (A. Zhou & Yuan, 2022). Medical resources lean toward clinical treatments during events such as the Ebola outbreak in West Africa and the COVID-19 pandemic, and at those times psychological services often become less accessible, which leads to a need to gain insight regarding mental health protective factors, such as personal resources and organizational support, to avoid noncombat attrition.
Anxiety is a serious psychological issue among Chinese military service members (Zhang et al., 2020). A meta-analysis of changes in the level of anxiety among Chinese military personnel showed a consistently rising tendency over time (Yang et al., 2014). As well as the problems of degraded military effectiveness, low morale, and higher incidence of violence, in the face of possible noncombat attrition it is essential to consider precautionary measures for mental health care of the military. Extensive research has shown that as a psychological resource, resilience can mitigate the likelihood of experiencing mental health issues (Bartone et al., 2012, 2016; Thomassen et al., 2015; Ureña et al., 2020; Wooten, 2012). In the context of the military, it has been found that as stress levels increase, the protective effect of resilience becomes more pronounced in dealing actively with stressful events (Bartone, 1999; Bartone et al., 2015; Sandvik et al., 2013) and reducing the severity of depression, anxiety, and substance abuse (Bartone et al., 2012; Hoopsick et al., 2019). A recent study showed that resilience had a stronger protective effect on the anxiety, depression, and likelihood of development of posttraumatic stress disorder of soldiers who had never been deployed, compared to those who had been previously deployed (Hoopsick et al., 2021). Considering this, we proposed the following hypothesis:
Hypothesis 1: The anxiety levels of new military recruits will be inversely related to their resilience.
In conservation of resources theory (Hobfoll, 1989, 2012), resilience is defined as a state of abundance in psychological and social resources, providing security and protection to individuals and promoting resource growth. Social support is a fundamental element that individuals use to navigate stressful situations and life events, and often plays a key role in their adaptation to new environments (Lau et al., 2018; Yakobi et al., 2022). This means that those individuals with higher levels of resilience are more likely to adopt coping mechanisms such as social support, which are beneficial in facing difficulties and setbacks and adapting to stressful situations. Resilience and social support are both considered to be protective factors for mental health and operate as positive contributors to adapting well to adversity and posttraumatic growth (Hu et al., 2022; Rakesh et al., 2022; Xu et al., 2022). Studies conducted with organizational members, with people receiving hemodialysis, with caregivers of people receiving hematopoietic stem cell transplantation, and with caregivers of people being treated for schizophrenia have all revealed a positive correlation between resilience and social support (Köse et al., 2021; Luo et al., 2020; Peng et al., 2022; Wu et al., 2021). Researchers have reported positive effects of resilience through social support on the psychological well-being of students (Malkoç & Yalçin, 2015) and on the health-related quality of life of women newly diagnosed with breast cancer (K. Zhou et al., 2022). Russell et al. (2016) also found that social support enhances the mental health and lowers the risk of psychological disorders among U.S. Army Special Operations personnel. In another study conducted with personnel involved in military operations, the results showed that social support can mitigate the harmful consequences of combat experiences (Reed‐Fitzke & Lucier‐Greer, 2020), making individuals less likely to suffer from posttraumatic stress disorder or commit suicide (Griffith, 2012). In closed barracks, new military recruits are separated from their families and other social relationships, making organizational support their most critical social support resource (Yakobi et al., 2022). Consequently, we put forward the second hypothesis:
Hypothesis 2: Social support will mediate the association between resilience and anxiety levels among new military recruits.
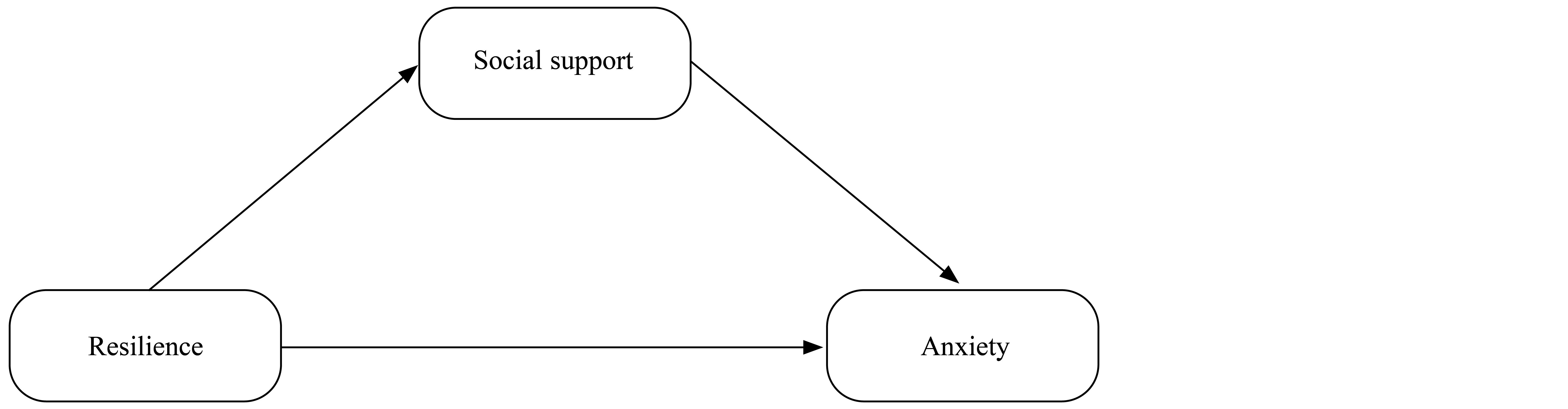
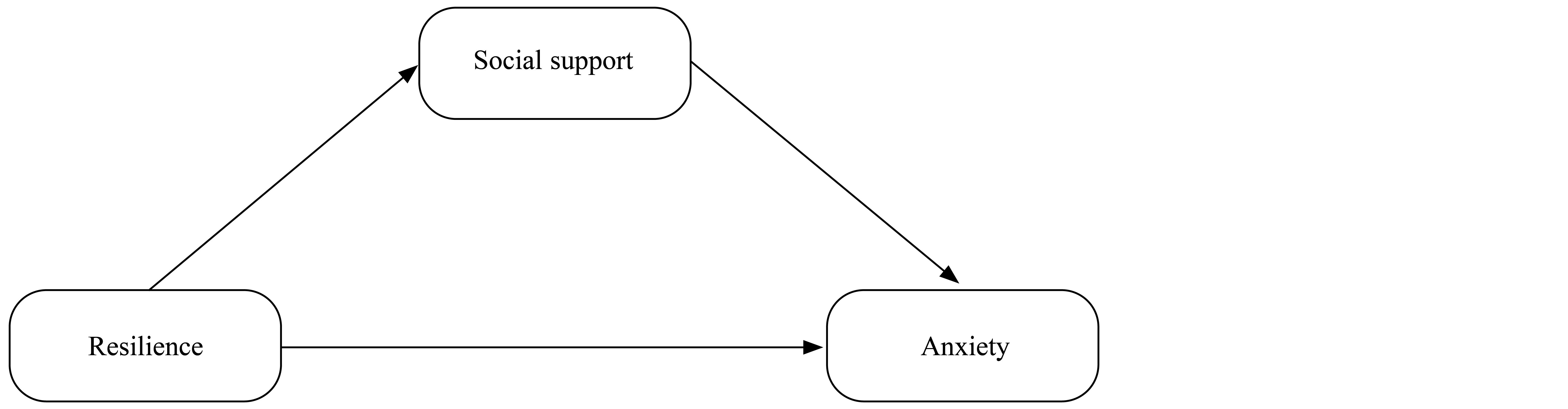
The conceptual model utilized in this study is set out in Figure 1.
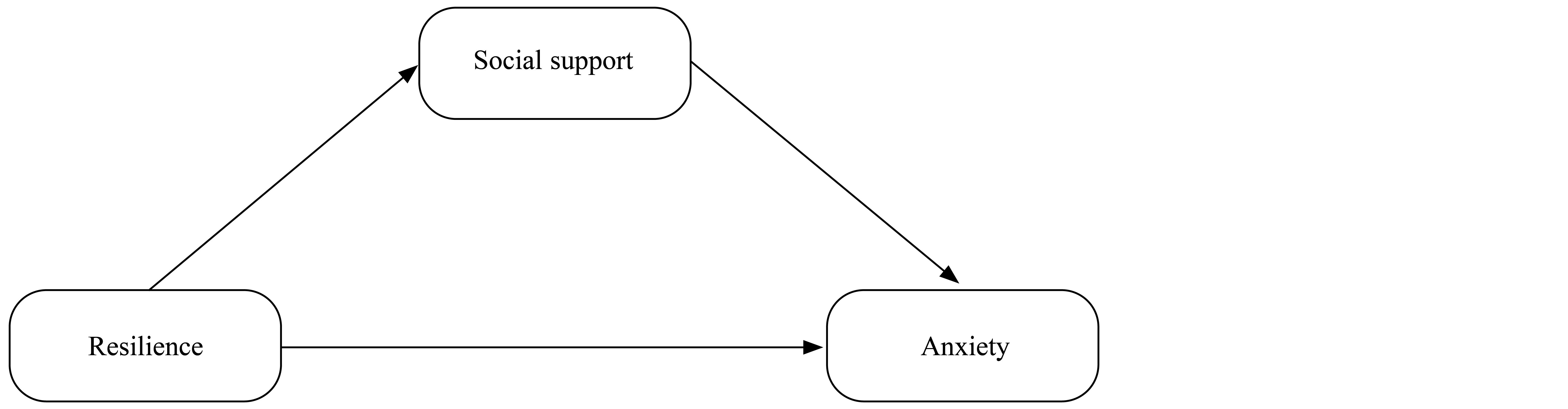
Figure 1. Conceptual Model
Method
Participants
The participants in this study were 724 compulsory servicemen with the rank of private in grassroots units, who participated in a routine assessment to ensure that their psychological status at the time was acceptable for the military environment and job requirements. After respondents were made aware of the objectives of the study, we received completed 717 survey forms. The final sample comprised 665 new recruits (635 men and 30 women).
Measures
Demographics
We first collected demographic data on gender, age, educational background, and place of upbringing.
Resilience
Psychological resilience was evaluated using the Connor-Davidson Resilience Scale (Connor & Davidson, 2003), which comprises 25 items (e.g., “Even when things look hopeless, I don’t give up”). Items are rated on a 5-point Likert scale where 0 = completely false, 1 = rarely true, 2 = occasionally true, 3 = often true, and 4 = almost always true. Total scores range from 0 to 100 points, with higher scores indicating greater resilience. Cronbach’s alpha in this study was .93.
Anxiety
The seven-item Generalized Anxiety Disorder Scale was used to assess anxiety (Spitzer et al., 2006). This scale is designed to assess how often individuals have been bothered by seven problems, including feeling nervous and worried (e.g., “Worrying too much about different things”), over the past 2 weeks. Items are rated on a 3-point Likert scale where 0 = not at all, 1 = for a few days, 2 = over half of the time, 3 = practically every day. Total scores range between 0 and 21, with higher ratings indicating more severe anxiety. Cronbach’s alpha in this study was .91.
Social Support
The 10-item Social Support Rating Scale was used to assess three dimensions of social support (Hou et al., 2020; Xiao, 1994): subjective support, objective support, and utilization of support. Four items are used to assess subjective support, including the individual’s emotional experience and satisfaction with receiving respect, support, and being understood by society (e.g., “What is the number of close friends that you rely on for support and assistance?”). Items are rated on a 4-point Likert scale where 1 = none, 2 = one–two, 3 = three–five, 4 = six or more. The objective support dimension comprises three items assessing concrete or useful/worthwhile aid, including direct material help, community relations, and group participation (e.g., “When encountering urgent situations, what sources of financial support and help do you receive?”). Response options are 1 = none or 2 = choose option(s) from sources below: A. Spouse, B. Other family members, C. Relatives, E. Colleagues, F. Workplace, G. Official or semiofficial organizations such as parties and unions, H. Unofficial organizations such as religious and social groups, I. Others (please list). The support utilization dimension, which includes three items, measures individuals’ active use of diverse forms of social support, including the manner of communicating, help seeking, and activity participation (e.g., “If you are faced with a difficult situation, who will you rely on?”). Items are rated on a 4-point Likert scale where 1 = no one, 2 = only one or two close friends, 3 = only when my friends ask me will I tell them my troubles, 4 = I will take the initiative to find someone to talk to about my troubles. Total scores range between 12 and 66, with higher scores indicating more social support. In this study Cronbach’s alpha was .73.
Data Analysis
Analysis of the data was conducted using SPSS 23.0 and Amos 24.0. To investigate the relationships among anxiety, social support, and resilience, we performed a Pearson’s correlation analysis.
Results
Descriptive Statistics and Correlation Analysis
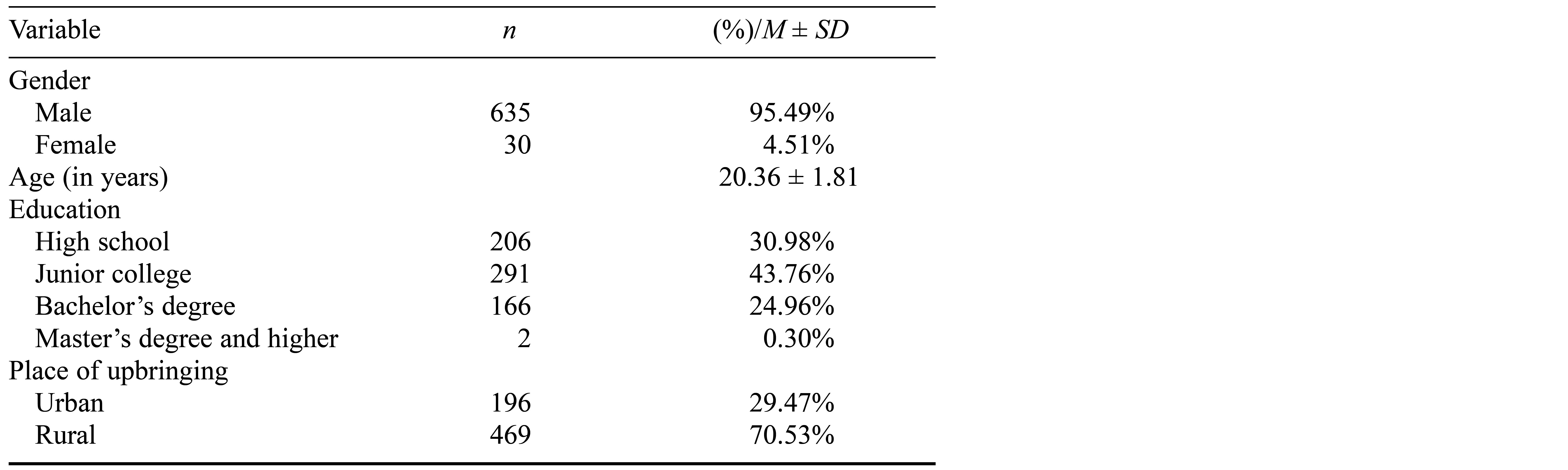
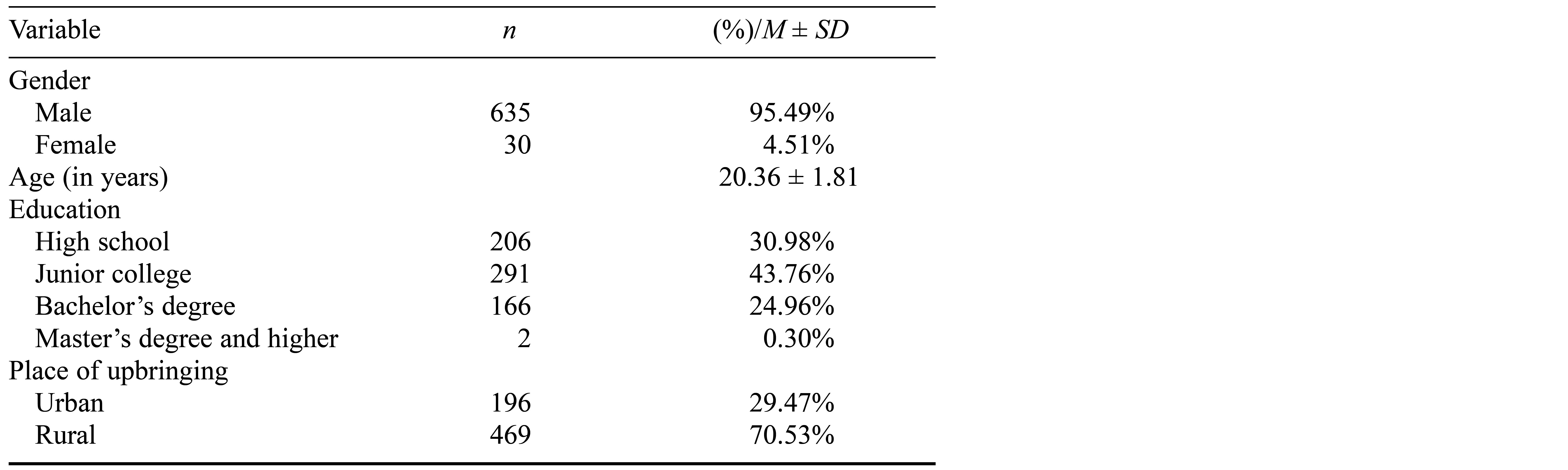
The sociodemographic characteristics of the participants are presented in Table 1. Most of the participants in this study were men. The average age of participants was 20.36 years (SD = 1.81, range = 18–25). In terms of education, more than half of the participants had attended junior college or had a higher educational qualification (69.02%), and just over 70% of them had grown up in a rural area.
Table 1. Descriptive Statistics of the Participants
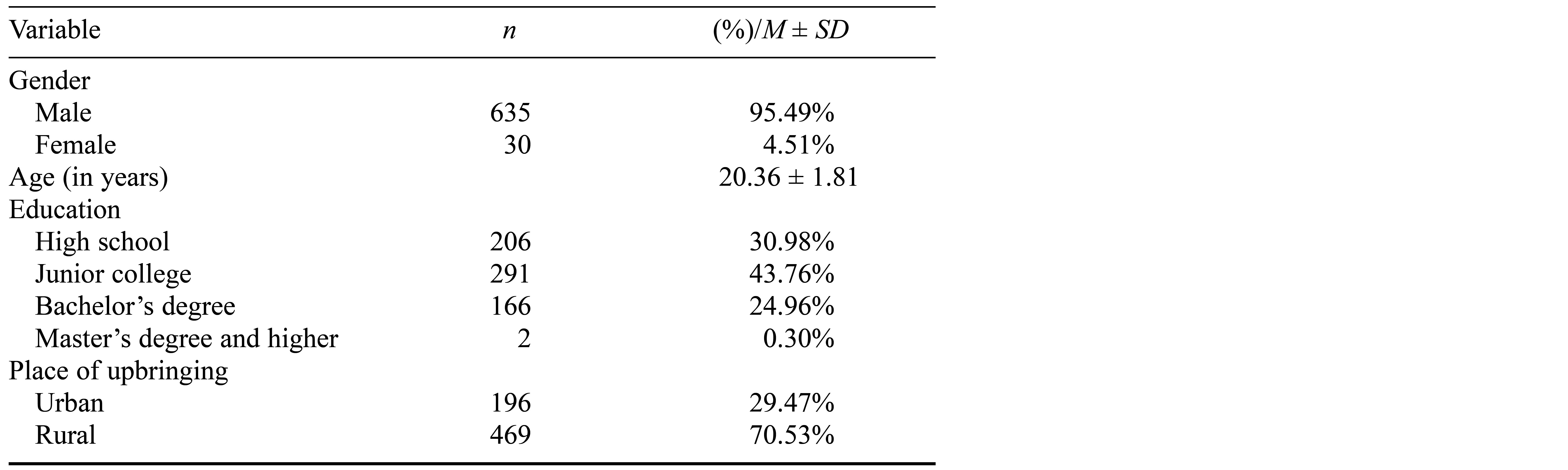
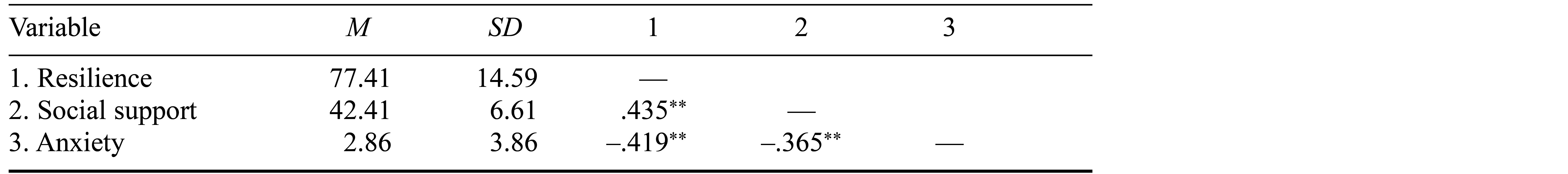
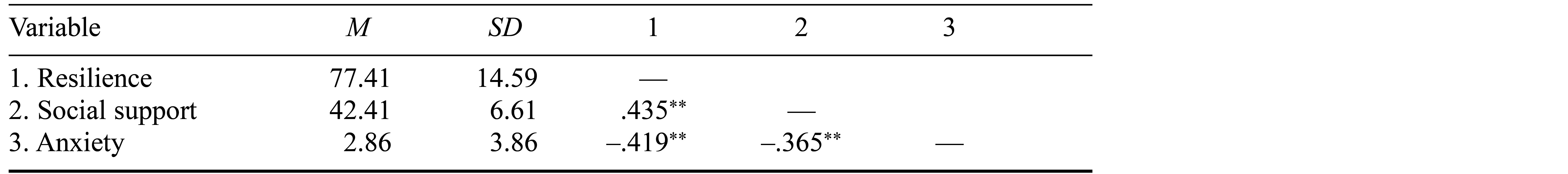
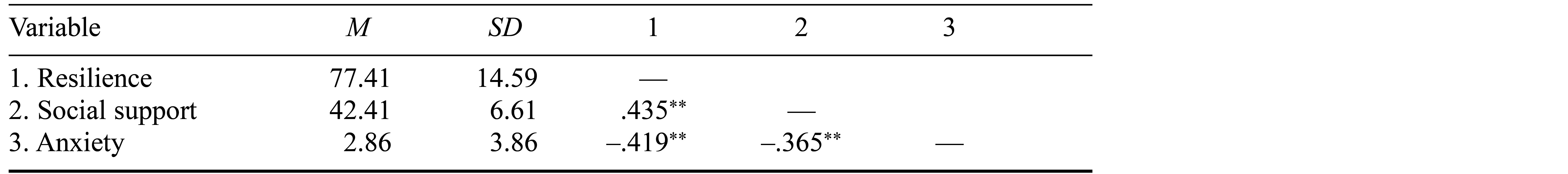
Table 2 presents the results of the correlation analyses. Social support and resilience showed a significantly positive association. A negative correlation was found between resilience and anxiety and, likewise, social support was negatively correlated with anxiety. Thus, Hypothesis 1 was supported.
Table 2. Correlations and Descriptive Statistics
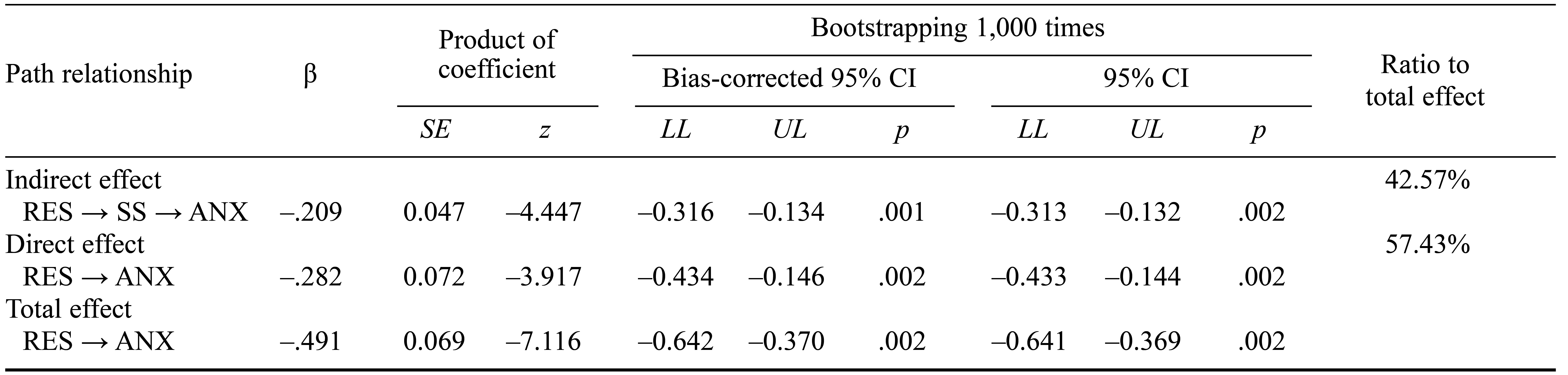
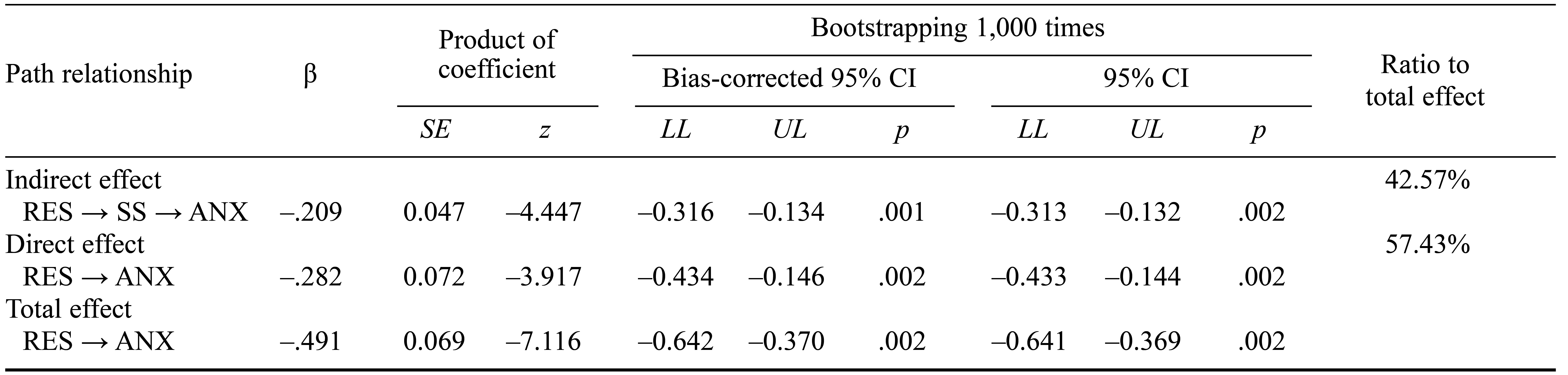
Test for Mediating Effect
We conducted a bootstrapping analysis with 1,000 resamples to evaluate the role of social support in mediating the relationship between resilience and anxiety (Baron & Kenny, 1986; Hayes, 2009). Detailed results are presented in Table 3. Resilience had a significant impact on social support, and social support had a significant influence on anxiety. Zero was not included in the bias-corrected 95% confidence interval or percentile 95% confidence interval for the indirect, direct, and total effects, indicating that these effects were all significant. Therefore, the relationship between resilience and anxiety was partially mediated by social support, and the indirect effect accounted for 42.57% of the variance. These results supported Hypothesis 2.
Table 3. Bootstrapping Analysis of the Mediating Effect of Social Support in the Relationship Between Resilience and Anxiety
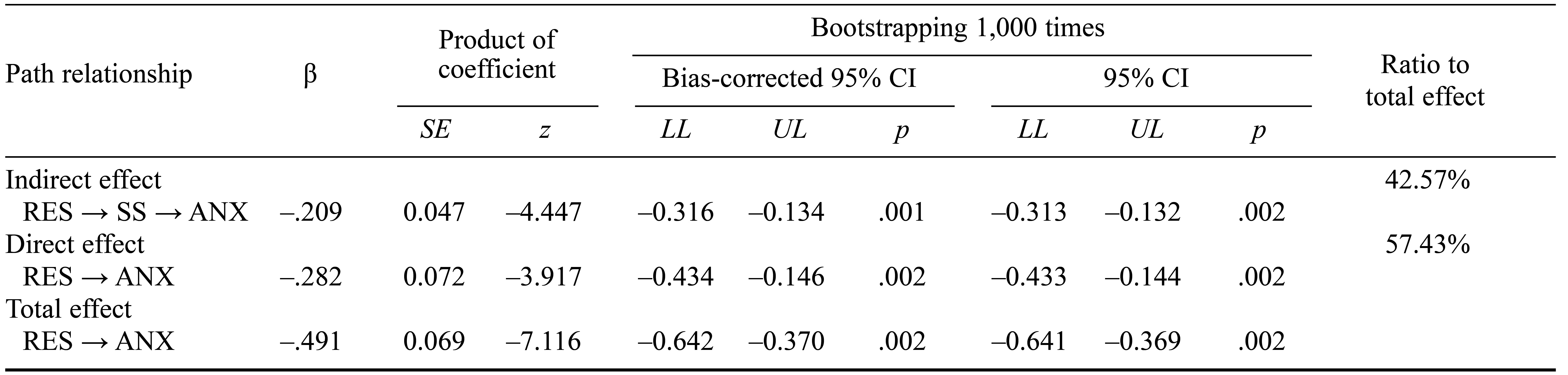
Note. RES = resilience; SS = social support; ANX = anxiety; CI = confidence interval; LL = lower limit; UL = upper limit.
Discussion
Socioeconomically, the COVID-19 pandemic has been detrimental to people’s mental health and well-being. Because of long-term quarantine policies and fear of infection, many people have experienced diverse psychological challenges (Brodhead, 2020; “COVID-19 and Mental Health,” 2021). Most new military recruits in China are in their early twenties, which is an age at which the early stages of severe mental illness often manifest (Bellivier et al., 2003; Rajji et al., 2009). We developed a mediating model to explain the influences of internal and external resources on the anxiety levels of new recruits. We found that resilience and social support are significantly and inversely related to anxiety, and that social support mediates the effect of internal resource protection on anxiety. This verification is fundamental to the army’s organizational support during the COVID-19 pandemic. The primary mission of the force is military training and operations, and the quarantine policy has already posed a major management challenge during the pandemic, so that it is crucial to prevent psychological disturbances from escalating into psychological disorders in order to guarantee the completion of primary missions, which will then reduce the cost effectiveness of military operations (Rahmani et al., 2018; Thomas et al., 2018).
Theoretical and Practical Implications
Mental illnesses are more likely to develop in military environments than in civilian environments because of high stress (Castro & Kintzle, 2014). Military personnel are challenged by anxiety, depression, and even suicide because of the stress caused by constant pressure (Pan et al., 2017). The data we collected and analyzed during the research process provide evidence that resilience and social support are reliable protective factors for new recruits’ mental health during the adaptation phase. In the military population, resilience and social support resources from families and the organization play vital roles in preventing anxiety, depression, and posttraumatic stress disorder (Griffith, 2012; Hoopsick et al., 2021; Waddell et al., 2023). Social support is an intermediary element fundamental to the adaptation process, well-being, and help-seeking behavior of servicemen and veterans (Waddell et al., 2023; Weir et al., 2019). However, new recruits in closed barracks are separated from their families and other social relationships, making organizational support their most critical social support resource. The aims of organizational support are to establish new military recruits’ external and internal resources through life guidance, resilience improvement programs, and timely psychological services. This includes the support of special interpersonal relationships in the barracks, where superiors must be responsible for subordinates. Counselors give professional psychological assessments and psychological services, training masters give professional guidance on daily training, and administrative masters are concerned with family relationships and personal growth. In the military environment, such support is both spontaneous and culturally driven.
Our study has confirmed that individuals can actively manage stress if they have good resilience and social support (Bartone, 1999; Bartone et al., 2012, 2015; Hoopsick et al., 2019; Sandvik et al., 2013), which provides suggestions for strategies to prevent mental health problems in the army. However, mental health issues are often viewed as private and personal, and help seeking is stigmatized within such cultures (Hom et al., 2017; Roscoe, 2020). Scholars have reported finding that perceived social support within the unit may even be associated with reluctance to seek the professional help that is available in the form of professional psychological assessments, group psychological training, counseling, and links to clinical resources. In particular, especially for those with severe mental illnesses, administrative barriers discourage help seeking, such as concern that seeking help may have negative implications for one’s military career (Hom et al., 2017; Russell et al., 2022; Schneider et al., 2022). Given that the stigmatization of psychological disorders may reduce help-seeking behaviors, we suggest regular psychological assessments, especially longitudinal evaluations. At the same time, projects to improve individuals’ resilience can be carried out as early as possible to minimize the occurrence of mental illness. Psychological services that help with instituting such a culture include psychological testing, mental health education, and group counseling. However, these services are not yet spread nationwide, so that advocacy remains important.
Limitations and Future Research Directions
Our study has several limitations. First, data were collected at a fixed time and the results reflect recruits’ psychological state only during military training. We did not monitor the recruits after they were assigned to different companies. In future research, military recruits’ psychological changes and causality patterns should be investigated using both longitudinal and experimental approaches. Second, compulsory soldiers account for the largest proportion of personnel in grassroots units, most of whom are new military recruits. However, for new military recruits, compulsory service usually lasts for 2 years, and they then have the right to choose whether to continue serving. This may explain the low anxiety scores observed in this study. The service period of noncommissioned officers (5 years) and also of cadres is much longer than that of compulsory soldiers, and may lead to more significant mental health risks. Therefore, it will be necessary to include these two groups in future studies. Finally, future studies could be conducted to consider how to advocate for a military culture in which the mental health of personnel is maintained, and to find ways to expand sources of support for military personnel to outside their unit (Peck & Parcell, 2021).
References
Baron, R. M., & Kenny, D. A. (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182.
Bartone, P. T. (1999). Hardiness protects against war-related stress in Army Reserve forces. Consulting Psychology Journal: Practice and Research, 51(2), 72–82.
Bartone, P. T., Hystad, S. W., Eid, J., & Brevik, J. I. (2012). Psychological hardiness and coping style as risk/resilience factors for alcohol abuse. Military Medicine, 177(5), 517–524.
Bartone, P. T., Johnsen, B. H., Eid, J., Hystad, S. W., & Laberg, J. C. (2016). Hardiness, avoidance coping, and alcohol consumption in war veterans: A moderated-mediation study. Stress & Health, 33(5), 498–507.
Bartone, P. T., Valdes, J. J., & Sandvik, A. (2015). Psychological hardiness predicts cardiovascular health. Psychology, Health & Medicine, 21(6), 743–749.
Bellivier, F., Golmard, J.-L., Rietschel, M., Schulze, T. G., Malafosse, A., Preisig, M., … Leboyer, M. (2003). Age at onset in bipolar 1 affective disorder: Further evidence for three subgroups. American Journal of Psychiatry, 160(5), 999–1001.
Brodhead, F. (2020). Mental health effects of COVID-19. American Journal of Nursing, 120(11), 15.
Castro, C. A., & Kintzle, S. (2014). Suicides in the military: The post-modern combat veteran and the Hemingway effect. Current Psychiatry Reports, 16(8), Article 460.
Clemons, E. P. (1996). Monitoring anxiety levels and coping skills among military recruits. Military Medicine, 161(1), 18–21.
Conner, K. R., McCarthy, M. D., Bajorska, A., Caine, E. D., Tu, X. M., & Knox, K. L. (2012). Mood, anxiety, and substance-use disorders and suicide risk in a military population cohort. Suicide and Life-Threatening Behavior, 42(6), 699–708.
Connor, K. M., & Davidson, J. R. T. (2003). Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety, 18(2), 76–82.
COVID-19 and Mental Health. (2021). Editorial. The Lancet Psychiatry, 8(2), 87.
Griffith, J. (2012). Suicide and war: The mediating effects of negative mood, posttraumatic stress disorder symptoms, and social support among Army National Guard soldiers. Suicide and Life-Threatening Behavior, 42(4), 453–469.
Hayes, A. F. (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76(4), 408–420.
Hobfoll, S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44(3), 513–524.
Hobfoll, S. E. (2012). Conservation of resources theory: Its implication for stress, health and resilience. In S. Folkman (Ed.), The Oxford handbook of stress, health and coping (pp. 127–147). Oxford University Press.
Hom, M. A., Stanley, I. H., Schneider, M. E., & Joiner, T. E., Jr. (2017). A systematic review of help-seeking and mental health service utilization among military service members. Clinical Psychology Review, 53, 59–78.
Hoopsick, R. A., Benson, K. R., Homish, D. L., & Homish, G. G. (2019). Resiliency factors that protect against post-deployment drug use among male US Army Reserve and National Guard soldiers. Drug and Alcohol Dependence, 199, 42–49.
Hoopsick, R. A., Homish, D. L., Collins, R. L., Nochajski, T. H., Read, J. P., Bartone, P. T., & Homish, G. G. (2021). Resilience to mental health problems and the role of deployment status among U.S. Army Reserve and National Guard soldiers. Social Psychiatry and Psychiatric Epidemiology, 56(7), 1299–1310.
Hou, T., Zhang, T., Cai, W., Song, X., Chen, A., Deng, G., & Ni, C. (2020). Social support and mental health among health care workers during Coronavirus disease 2019 outbreak: A moderated mediation model. PLOS ONE, 15(5), Article e0233831.
Hu, J., Huang, Y., Liu, J., Zheng, Z., Xu, X., Zhou, Y., & Wang, J. (2022). COVID-19 related stress and mental health outcomes 1 year after the peak of the pandemic outbreak in China: The mediating effect of resilience and social support. Frontiers in Psychiatry, 13, Article 828379.
Köse, S., Baykal, B., & Bayat, İ. K. (2021). Mediator role of resilience in the relationship between social support and work life balance. Australian Journal of Psychology, 73(3), 316–325.
Lau, E. Y. H., Chan, K. K. S., & Lam, C. B. (2018). Social support and adjustment outcomes of first-year university students in Hong Kong: Self-esteem as a mediator. Journal of College Student Development, 59(1), 129–134.
Lucier‐Greer, M., Frye‐Cox, N., Reed‐Fitzke, K., Ferraro, A. J., & Mancini, J. A. (2022). Military‐related stress, self‐efficacy, and anxiety: Investigating the role of marital quality in military couples. Family Process. Advance online publication.
Luo, R.-Z., Zhang, S., & Liu, Y.-H. (2020). Short report: Relationships among resilience, social support, coping style and posttraumatic growth in hematopoietic stem cell transplantation caregivers. Psychology, Health & Medicine, 25(4), 389–395.
Malkoç, A., & Yalçin, İ. (2015). Relationships among resilience, social support, coping, and psychological well-being among university students. Turkish Psychological Counseling and Guidance Journal, 5(43), 35–43.
Markovitz, P. J. (1993). Treatment of anxiety in the elderly. The Journal of Clinical Psychiatry, 54, 64–68.
Pan, Y., Cai, W., Dong, W., Xiao, J., Yan, J., & Cheng, Q. (2017). Behavior characteristics of the attention network of military personnel with high and low trait anxiety. Medicine, 96(17), Article e6630.
Peck, B. S., & Parcell, E. S. (2021). Talking about mental health: Dilemmas U.S. military service members and spouses experience post deployment. Journal of Family Communication, 21(2), 90–106.
Peng, L., Ye, Y., Wang, L., Qiu, W., Huang, S., Wang, L., … Lin, J. (2022). Chain mediation model of perceived stress, resilience, and social support on coping styles of Chinese patients on hemodialysis during COVID-19 pandemic lockdown. Medical Science Monitor, 28, Article e935300.
Rahmani, J., Milajerdi, A., & Dorosty-Motlagh, A. (2018). Association of the Alternative Healthy Eating Index (AHEI-2010) with depression, stress and anxiety among Iranian military personnel. BMJ Military Health, 164(2), 87–91.
Rajji, T. K., Ismail, Z., & Mulsant, B. H. (2009). Age at onset and cognition in schizophrenia: Meta-analysis. The British Journal of Psychiatry, 195(4), 286–293.
Rakesh, G., Clausen, A. N., Buckley, M. N., Clarke-Rubright, E., Fairbank, J. A., … Morey, R. A. (2022). The role of trauma, social support, and demography on veteran resilience. European Journal of Psychotraumatology, 13(1), Article 2058267.
Reed‐Fitzke, K., & Lucier‐Greer, M. (2020). The buffering effect of relationships on combat exposure, military performance, and mental health of U.S. military soldiers: A vantage point for CFTs. Journal of Marital and Family Therapy, 46(2), 321–336.
Roscoe, R. A. (2020). The battle against mental health stigma: Examining how veterans with PTSD communicatively manage stigma. Health Communication, 36(11), 1378–1387.
Russell, D. W., Benedek, D. M., Naifeh, J. A., Fullerton, C. S., Benevides, N., Ursano, R. J., … Cacciopo, J. T. (2016). Social support and mental health outcomes among U.S. Army Special Operations personnel. Military Psychology, 28(6), 361–375.
Russell, D. W., Russell, C. A., & Hill, R. P. (2022). Mental health service utilization after military missions: The double-edged consequences of unit-level organizational support. Psychological Services, 19(Suppl 2), 113–125.
Sandvik, A. M., Bartone, P. T., Hystad, S. W., Phillips, T. M., Thayer, J. F., & Johnsen, B. H. (2013). Psychological hardiness predicts neuroimmunological responses to stress. Psychology, Health & Medicine, 18(6), 705–713.
Schneider, M., Werner, S., Yavnai, N., Ben Yehuda, A., & Shelef, L. (2022). Israeli soldiers’ intentions and actions toward seeking mental health help: Barriers and facilitators. Journal of Clinical Psychology, 79(2), 449–465.
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
Surtees, P. G., & Wainwright, N. W. (1996). Fragile states of mind: Neuroticism, vulnerability and the long-term outcome of depression. British Journal of Psychiatry, 169(3), 338–347.
Thomas, J. L., Adrian, A. L., Wood, M. D., Crouch, C. L., Lee, J. D., & Adler, A. B. (2018). Mental health and stress among Army civilians, spouses, and soldiers in a closing military community. Armed Forces & Society, 45(4), 612–636.
Thomassen, Å. G., Hystad, S. W., Johnsen, B. H., Johnsen, G. E., Laberg, J. C., & Eid, J. (2015). The combined influence of hardiness and cohesion on mental health in a military peacekeeping mission: A prospective study. Scandinavian Journal of Psychology, 56(5), 560–566.
Ureña, S., Taylor, M. G., & Carr, D. C. (2020). The impact of military service exposures and psychological resilience on the mental health trajectories of older male veterans. Journal of Aging and Health, 33(3–4), 237–248.
Waddell, E., Rioseco, P., Van Hooff, M., Daraganova, G., Lawrence, D., Rikkers, W., … Lawn, S. (2023). Families’ experiences of supporting Australian veterans to seek help for a mental health problem: A linked data analysis of national surveys with families and veterans. Journal of Mental Health. Advance online publication.
Weir, B., Cunningham, M., Abraham, L., & Allanson-Oddy, C. (2019). Military veteran engagement with mental health and well-being services: A qualitative study of the role of the peer support worker. Journal of Mental Health, 28(6), 647–653.
Wooten, N. R. (2012). Deployment cycle stressors and post-traumatic stress symptoms in Army National Guard women: The mediating effect of resilience. Social Work in Health Care, 51(9), 828–849.
Wu, C., Liu, Y., Ma, S., Jing, G., Zhou, W., Qu, L., … Wu, Y. (2021). The mediating roles of coping styles and resilience in the relationship between perceived social support and posttraumatic growth among primary caregivers of schizophrenic patients: A cross-sectional study. BMC Psychiatry, 21(1), Article 58.
Wynn, G., Morganstein, J. C., Jetly, R., Ford, S. C., Vance, M. C., Meyer, E. G., … Ursano, R. J. (2020). Military mental health and COVID-19. Journal of Military, Veteran and Family Health, 6(S2), 21–26.
Xiao, S. Y. (1994). The theoretical basis and research application of Social Support Rating Scale. Journal of Clinical Psychiatry, 4(2), 98–100.
Xu, C., Wang, Y., Wang, Z., Li, B., Yan, C., Zhang, S., … Peng, J. (2022). Social support and coping style of medical residents in China: The mediating role of psychological resilience. Frontiers in Psychiatry, 13, Article 888024.
Yakobi, M., Dekel, R., Yavnai, N., Ben Yehuda, A., & Shelef, L. (2022). Contributing factors to Israeli soldiers’ adaptation to military noncombat positions. Military Medicine,188(7–8), e1981–e1989.
Yang, Z., Cao, F., Lu, H., Zhu, X., & Miao, D. (2014). Changes of anxiety in Chinese military personnels over time: A cross-temporal meta-analysis. International Journal of Mental Health Systems, 8, Article 19.
Zhang, F., Zhang, X., Mao, X., Chen, A., Yin, Q., & Deng, G. (2020). Interpretation bias of high trait anxiety Chinese military servicemen in ambiguous military scenarios. Medicine, 99(3), Article e18746.
Zhou, A., & Yuan, Y. (2022). Aggression and anxiety influence the relationship between interpersonal sensitivity and military morale among new recruits. Social Behavior and Personality: An international journal, 50(7), Article 11668.
Zhou, K., Ning, F., Wang, X., Wang, W., Han, D., & Li, X. (2022). Perceived social support and coping style as mediators between resilience and health-related quality of life in women newly diagnosed with breast cancer: A cross-sectional study. BMC Women’s Health, 22(1), Article 198.
Baron, R. M., & Kenny, D. A. (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182.
Bartone, P. T. (1999). Hardiness protects against war-related stress in Army Reserve forces. Consulting Psychology Journal: Practice and Research, 51(2), 72–82.
Bartone, P. T., Hystad, S. W., Eid, J., & Brevik, J. I. (2012). Psychological hardiness and coping style as risk/resilience factors for alcohol abuse. Military Medicine, 177(5), 517–524.
Bartone, P. T., Johnsen, B. H., Eid, J., Hystad, S. W., & Laberg, J. C. (2016). Hardiness, avoidance coping, and alcohol consumption in war veterans: A moderated-mediation study. Stress & Health, 33(5), 498–507.
Bartone, P. T., Valdes, J. J., & Sandvik, A. (2015). Psychological hardiness predicts cardiovascular health. Psychology, Health & Medicine, 21(6), 743–749.
Bellivier, F., Golmard, J.-L., Rietschel, M., Schulze, T. G., Malafosse, A., Preisig, M., … Leboyer, M. (2003). Age at onset in bipolar 1 affective disorder: Further evidence for three subgroups. American Journal of Psychiatry, 160(5), 999–1001.
Brodhead, F. (2020). Mental health effects of COVID-19. American Journal of Nursing, 120(11), 15.
Castro, C. A., & Kintzle, S. (2014). Suicides in the military: The post-modern combat veteran and the Hemingway effect. Current Psychiatry Reports, 16(8), Article 460.
Clemons, E. P. (1996). Monitoring anxiety levels and coping skills among military recruits. Military Medicine, 161(1), 18–21.
Conner, K. R., McCarthy, M. D., Bajorska, A., Caine, E. D., Tu, X. M., & Knox, K. L. (2012). Mood, anxiety, and substance-use disorders and suicide risk in a military population cohort. Suicide and Life-Threatening Behavior, 42(6), 699–708.
Connor, K. M., & Davidson, J. R. T. (2003). Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety, 18(2), 76–82.
COVID-19 and Mental Health. (2021). Editorial. The Lancet Psychiatry, 8(2), 87.
Griffith, J. (2012). Suicide and war: The mediating effects of negative mood, posttraumatic stress disorder symptoms, and social support among Army National Guard soldiers. Suicide and Life-Threatening Behavior, 42(4), 453–469.
Hayes, A. F. (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76(4), 408–420.
Hobfoll, S. E. (1989). Conservation of resources: A new attempt at conceptualizing stress. American Psychologist, 44(3), 513–524.
Hobfoll, S. E. (2012). Conservation of resources theory: Its implication for stress, health and resilience. In S. Folkman (Ed.), The Oxford handbook of stress, health and coping (pp. 127–147). Oxford University Press.
Hom, M. A., Stanley, I. H., Schneider, M. E., & Joiner, T. E., Jr. (2017). A systematic review of help-seeking and mental health service utilization among military service members. Clinical Psychology Review, 53, 59–78.
Hoopsick, R. A., Benson, K. R., Homish, D. L., & Homish, G. G. (2019). Resiliency factors that protect against post-deployment drug use among male US Army Reserve and National Guard soldiers. Drug and Alcohol Dependence, 199, 42–49.
Hoopsick, R. A., Homish, D. L., Collins, R. L., Nochajski, T. H., Read, J. P., Bartone, P. T., & Homish, G. G. (2021). Resilience to mental health problems and the role of deployment status among U.S. Army Reserve and National Guard soldiers. Social Psychiatry and Psychiatric Epidemiology, 56(7), 1299–1310.
Hou, T., Zhang, T., Cai, W., Song, X., Chen, A., Deng, G., & Ni, C. (2020). Social support and mental health among health care workers during Coronavirus disease 2019 outbreak: A moderated mediation model. PLOS ONE, 15(5), Article e0233831.
Hu, J., Huang, Y., Liu, J., Zheng, Z., Xu, X., Zhou, Y., & Wang, J. (2022). COVID-19 related stress and mental health outcomes 1 year after the peak of the pandemic outbreak in China: The mediating effect of resilience and social support. Frontiers in Psychiatry, 13, Article 828379.
Köse, S., Baykal, B., & Bayat, İ. K. (2021). Mediator role of resilience in the relationship between social support and work life balance. Australian Journal of Psychology, 73(3), 316–325.
Lau, E. Y. H., Chan, K. K. S., & Lam, C. B. (2018). Social support and adjustment outcomes of first-year university students in Hong Kong: Self-esteem as a mediator. Journal of College Student Development, 59(1), 129–134.
Lucier‐Greer, M., Frye‐Cox, N., Reed‐Fitzke, K., Ferraro, A. J., & Mancini, J. A. (2022). Military‐related stress, self‐efficacy, and anxiety: Investigating the role of marital quality in military couples. Family Process. Advance online publication.
Luo, R.-Z., Zhang, S., & Liu, Y.-H. (2020). Short report: Relationships among resilience, social support, coping style and posttraumatic growth in hematopoietic stem cell transplantation caregivers. Psychology, Health & Medicine, 25(4), 389–395.
Malkoç, A., & Yalçin, İ. (2015). Relationships among resilience, social support, coping, and psychological well-being among university students. Turkish Psychological Counseling and Guidance Journal, 5(43), 35–43.
Markovitz, P. J. (1993). Treatment of anxiety in the elderly. The Journal of Clinical Psychiatry, 54, 64–68.
Pan, Y., Cai, W., Dong, W., Xiao, J., Yan, J., & Cheng, Q. (2017). Behavior characteristics of the attention network of military personnel with high and low trait anxiety. Medicine, 96(17), Article e6630.
Peck, B. S., & Parcell, E. S. (2021). Talking about mental health: Dilemmas U.S. military service members and spouses experience post deployment. Journal of Family Communication, 21(2), 90–106.
Peng, L., Ye, Y., Wang, L., Qiu, W., Huang, S., Wang, L., … Lin, J. (2022). Chain mediation model of perceived stress, resilience, and social support on coping styles of Chinese patients on hemodialysis during COVID-19 pandemic lockdown. Medical Science Monitor, 28, Article e935300.
Rahmani, J., Milajerdi, A., & Dorosty-Motlagh, A. (2018). Association of the Alternative Healthy Eating Index (AHEI-2010) with depression, stress and anxiety among Iranian military personnel. BMJ Military Health, 164(2), 87–91.
Rajji, T. K., Ismail, Z., & Mulsant, B. H. (2009). Age at onset and cognition in schizophrenia: Meta-analysis. The British Journal of Psychiatry, 195(4), 286–293.
Rakesh, G., Clausen, A. N., Buckley, M. N., Clarke-Rubright, E., Fairbank, J. A., … Morey, R. A. (2022). The role of trauma, social support, and demography on veteran resilience. European Journal of Psychotraumatology, 13(1), Article 2058267.
Reed‐Fitzke, K., & Lucier‐Greer, M. (2020). The buffering effect of relationships on combat exposure, military performance, and mental health of U.S. military soldiers: A vantage point for CFTs. Journal of Marital and Family Therapy, 46(2), 321–336.
Roscoe, R. A. (2020). The battle against mental health stigma: Examining how veterans with PTSD communicatively manage stigma. Health Communication, 36(11), 1378–1387.
Russell, D. W., Benedek, D. M., Naifeh, J. A., Fullerton, C. S., Benevides, N., Ursano, R. J., … Cacciopo, J. T. (2016). Social support and mental health outcomes among U.S. Army Special Operations personnel. Military Psychology, 28(6), 361–375.
Russell, D. W., Russell, C. A., & Hill, R. P. (2022). Mental health service utilization after military missions: The double-edged consequences of unit-level organizational support. Psychological Services, 19(Suppl 2), 113–125.
Sandvik, A. M., Bartone, P. T., Hystad, S. W., Phillips, T. M., Thayer, J. F., & Johnsen, B. H. (2013). Psychological hardiness predicts neuroimmunological responses to stress. Psychology, Health & Medicine, 18(6), 705–713.
Schneider, M., Werner, S., Yavnai, N., Ben Yehuda, A., & Shelef, L. (2022). Israeli soldiers’ intentions and actions toward seeking mental health help: Barriers and facilitators. Journal of Clinical Psychology, 79(2), 449–465.
Spitzer, R. L., Kroenke, K., Williams, J. B., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
Surtees, P. G., & Wainwright, N. W. (1996). Fragile states of mind: Neuroticism, vulnerability and the long-term outcome of depression. British Journal of Psychiatry, 169(3), 338–347.
Thomas, J. L., Adrian, A. L., Wood, M. D., Crouch, C. L., Lee, J. D., & Adler, A. B. (2018). Mental health and stress among Army civilians, spouses, and soldiers in a closing military community. Armed Forces & Society, 45(4), 612–636.
Thomassen, Å. G., Hystad, S. W., Johnsen, B. H., Johnsen, G. E., Laberg, J. C., & Eid, J. (2015). The combined influence of hardiness and cohesion on mental health in a military peacekeeping mission: A prospective study. Scandinavian Journal of Psychology, 56(5), 560–566.
Ureña, S., Taylor, M. G., & Carr, D. C. (2020). The impact of military service exposures and psychological resilience on the mental health trajectories of older male veterans. Journal of Aging and Health, 33(3–4), 237–248.
Waddell, E., Rioseco, P., Van Hooff, M., Daraganova, G., Lawrence, D., Rikkers, W., … Lawn, S. (2023). Families’ experiences of supporting Australian veterans to seek help for a mental health problem: A linked data analysis of national surveys with families and veterans. Journal of Mental Health. Advance online publication.
Weir, B., Cunningham, M., Abraham, L., & Allanson-Oddy, C. (2019). Military veteran engagement with mental health and well-being services: A qualitative study of the role of the peer support worker. Journal of Mental Health, 28(6), 647–653.
Wooten, N. R. (2012). Deployment cycle stressors and post-traumatic stress symptoms in Army National Guard women: The mediating effect of resilience. Social Work in Health Care, 51(9), 828–849.
Wu, C., Liu, Y., Ma, S., Jing, G., Zhou, W., Qu, L., … Wu, Y. (2021). The mediating roles of coping styles and resilience in the relationship between perceived social support and posttraumatic growth among primary caregivers of schizophrenic patients: A cross-sectional study. BMC Psychiatry, 21(1), Article 58.
Wynn, G., Morganstein, J. C., Jetly, R., Ford, S. C., Vance, M. C., Meyer, E. G., … Ursano, R. J. (2020). Military mental health and COVID-19. Journal of Military, Veteran and Family Health, 6(S2), 21–26.
Xiao, S. Y. (1994). The theoretical basis and research application of Social Support Rating Scale. Journal of Clinical Psychiatry, 4(2), 98–100.
Xu, C., Wang, Y., Wang, Z., Li, B., Yan, C., Zhang, S., … Peng, J. (2022). Social support and coping style of medical residents in China: The mediating role of psychological resilience. Frontiers in Psychiatry, 13, Article 888024.
Yakobi, M., Dekel, R., Yavnai, N., Ben Yehuda, A., & Shelef, L. (2022). Contributing factors to Israeli soldiers’ adaptation to military noncombat positions. Military Medicine,188(7–8), e1981–e1989.
Yang, Z., Cao, F., Lu, H., Zhu, X., & Miao, D. (2014). Changes of anxiety in Chinese military personnels over time: A cross-temporal meta-analysis. International Journal of Mental Health Systems, 8, Article 19.
Zhang, F., Zhang, X., Mao, X., Chen, A., Yin, Q., & Deng, G. (2020). Interpretation bias of high trait anxiety Chinese military servicemen in ambiguous military scenarios. Medicine, 99(3), Article e18746.
Zhou, A., & Yuan, Y. (2022). Aggression and anxiety influence the relationship between interpersonal sensitivity and military morale among new recruits. Social Behavior and Personality: An international journal, 50(7), Article 11668.
Zhou, K., Ning, F., Wang, X., Wang, W., Han, D., & Li, X. (2022). Perceived social support and coping style as mediators between resilience and health-related quality of life in women newly diagnosed with breast cancer: A cross-sectional study. BMC Women’s Health, 22(1), Article 198.