Alcohol use disorder (AUD) is a condition that encompasses alcohol abuse and dependence and includes symptoms of alcohol cravings, mood dysregulation, increased stress response, and impulsive behavior (American Psychiatric Association, 2015). AUD is a pervasive public health problem with detrimental consequences for individuals, families, and society, resulting in car accidents, crimes, healthcare problems (e.g., suicide), and mental and physical health problems (Priddy et al., 2018; World Health Organization, 2018). Moreover, it is one of the most prevalent mental disorders worldwide, affecting 237 million men and 46 million women (World Health Organization, 2018). In the United States, the 1-year prevalence of AUD (i.e., the percentage of individuals with AUD at any point during a single year) is 13.9% and the lifetime prevalence of AUD (i.e., the percentage of individuals in a population who have ever experienced AUD over the course of their lifetime) is 29.1%. It has been shown that AUD is affected by marital status and socioeconomic status (Grant et al., 2015). Another study found that as of 2018, 5% of Americans aged 12 years and older had experienced AUD and nearly half of Americans met the AUD criteria on a lifetime basis (Tucker et al., 2020).
However, compared to AUD’s high prevalence, the rate of receiving or continuing specialized treatment is low, and the likelihood of AUD leading to other substance use disorders is high (Lee, 2019). Various effective treatments for AUD have been proposed to reduce social costs and improve quality of life. One meta-analysis presented examples of treatments for AUD, including cognitive behavioral therapy, motivational enhancement therapy, 12-step programs, Alcoholics Anonymous, meditation, stress management, social skills training, music therapy, and art therapy (S. A. Kim et al., 2015). Previous studies on risk factors have confirmed that AUD increases as a result of various psychological causes (Petit et al., 2015).
Specifically, dysregulation of moods is a strong emotional element and key factor in AUD (Jakubczyk et al., 2020). Mood regulation refers to strategies that affect when, how, and for how long certain emotions are experienced and expressed (Gross, 2014). Mood dysregulation contributes to depressive symptoms and sleep disturbances in general, worsening these symptoms (Brower, 2003; Palmer et al., 2018). Clinically, mood dysregulation is a characteristic AUD symptom (American Psychiatric Association, 2013; Gross, 2013). AUD is a coping strategy to relieve and avoid stress, and the higher the stress, the higher the possibility of AUD (Cavicchioli et al., 2018). In other words, increased mood dysregulation and stress responses are key to inducing negative mood states in the process of AUD treatment (Tang, Posner, et al., 2015).
Thus, successful treatment of AUD may depend on regulating negative mood states, such as anxiety, anger, and depression, which are major triggers for persistent alcohol use behavior (Carey & Correia, 1997). Indeed, many theories have focused on reducing negative moods about addiction and AUD (Baker et al., 2004; Cooper et al., 1995; Cox & Klinger, 1988; Khantzian, 1987). Neuroscience studies have shown that the anterior cingulate cortex and medial prefrontal cortex are brain structures related to mood regulation through the limbic system (Rudebeck et al., 2008). Mood dysregulation in people with AUD is related to decreased activity in the anterior cingulate cortex and medial prefrontal cortex (Tang, Posner, et al., 2015). In addition, regulating cravings and negative emotions in individuals with AUD is associated with the successful engagement of the prefrontal cortex (Suzuki et al., 2020). Therefore, it is possible to increase mood regulation and promote rehabilitation in clients with AUD by increasing activity in their anterior cingulate cortex and medial prefrontal cortex (Goldstein & Volkow, 2011; Tang, Posner, et al., 2015).
On the basis of the working principle of brain neuroscience, meditation training has been presented as one evidence-based method for controlling moods and reducing stress. Prior research has shown that mindfulness practice improves mood regulation and reduces stress (Cavicchioli et al., 2018). Besides that, psychosocial stress has been suggested as another area that meditation affects. Psychosocial stress refers to the stress experienced due to the interaction between psychological factors, like emotions and thoughts, and social factors, like environmental and societal conditions. One experimental study demonstrated a significant decrease in psychosocial stress in the meditation intervention group of people with AUD versus a slight increase in the control group (K. I. Kang, 2019). Another study on meditation training for people with AUD revealed an inverse correlation between stress (identified using the Perceived Stress Scale) and psychological distress (identified using the Kessler Psychological Distress Scale; Gryczynski et al., 2018).
Additionally, meditation has been utilized as an evidence-based treatment to improve mood regulation in clients with AUD (Hölzel et al., 2011). Meditation increases positive mood and decreases negative mood by integrating experiences through nonjudgmental concentration training (Tang, Hölzel, et al., 2015). Meditation training for clients with AUD improves mood regulation, reduces stress response, weakens the link between stress and addiction, and enhances self-regulation ability, thereby suppressing negative impulses and improving psychosocial well-being (Garland et al., 2014).
Regarding specific studies that have explored meditation training for AUD, S. H. Park and Lee (2016) provided a weekly meditation program for community clients with AUD for 10 weeks, including body scan, breathing meditation, loving–kindness meditation, walking meditation, yoga meditation, and short explanations regarding each week’s topic. Through these meditations, the participants learned not only to accept the present state as it is but also to allow it. Similarly, H. N. Park and Yu (2005) reported that mood stability in outpatient clients with AUD increased after a 6-week meditation training. A randomized control study investigating the brain science of meditation’s mood regulating effect reported that the brain imaging activity of the experimental group that received meditation training increased significantly compared to that of the control group (Tang, Hölzel, et al., 2015).
Furthermore, mindfulness training is a promising intervention option for preventing the recurrence of AUD (Chiesa & Serretti, 2014; Li et al., 2017). According to previous studies, mindfulness meditation to prevent alcohol-related substance use relapse is more effective than standard relapse prevention and also has a longer-lasting effect (Bowen et al., 2014). Additionally, mindfulness meditation training is known to be effective for treating AUD, is generally provided on a group basis, is structured as several weeks of intervention, and is comparable to the therapeutic effect of individual therapy (Garland & Howard, 2018).
However, most studies reporting that meditation training is an effective modality for managing negative emotions in AUD patients have been conducted outside of Korea. Moreover, evidence is scarce on meditation’s effect on mood regulation for inpatient clients with AUD in Korea, and we questioned whether the results of other studies would be the same for Korean participants. In particular, as our target study sample comprised actual clients admitted to hospitals, we believed that the results would be significant. Therefore, in this study we provided a meditation training program for inpatient clients with AUD and tested its efficacy as a treatment method for mood dysregulation and stress reduction. We formed the following hypotheses:
Hypothesis 1: The experimental group participating in inpatient meditation training for alcohol use disorder will report a greater reduction in psychosocial stress than will the control group.
Hypothesis 2: The experimental group participating in inpatient meditation training for alcohol use disorder will report a greater reduction in mood dysregulation than will the control group.
Method
Ethical Considerations
All procedures performed involving human participants were in accordance with the ethical standards of the Institutional Review Board of Chung-Ang University and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The participants voluntarily gave written consent after receiving a detailed explanation regarding the study’s purpose and process. They understood that they could withdraw from the study whenever they wanted to without any penalty and that the collected data would be managed confidentially and contained safely.
Research Design
This was a nonequivalent control group pre- and post-test experimental study to test the effects of group meditation on mood states and psychosocial stress in inpatient clients with AUD. There were two groups: the untreated control group and the experimental group, with the latter participating in the eight-session meditation training program in our study.
Participants
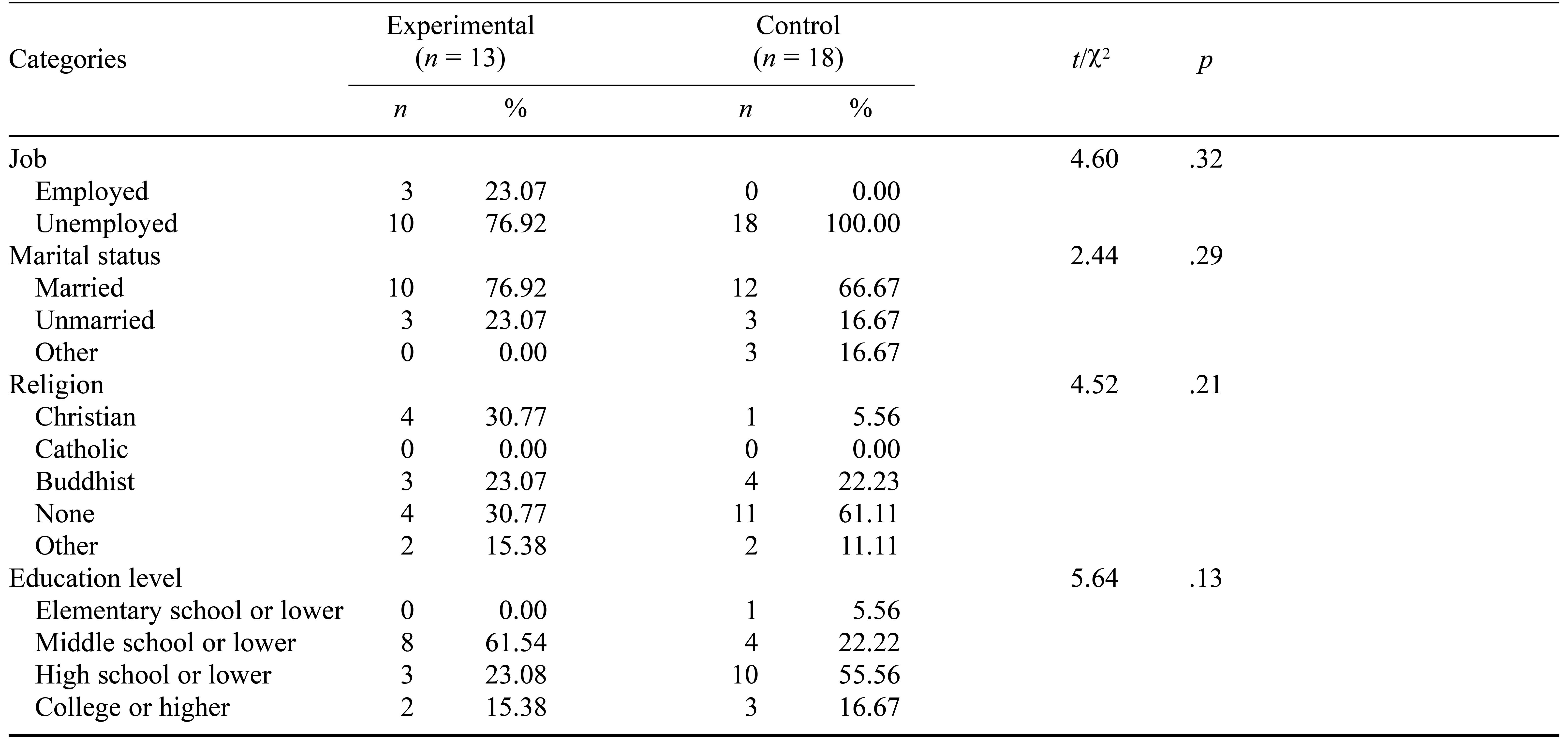
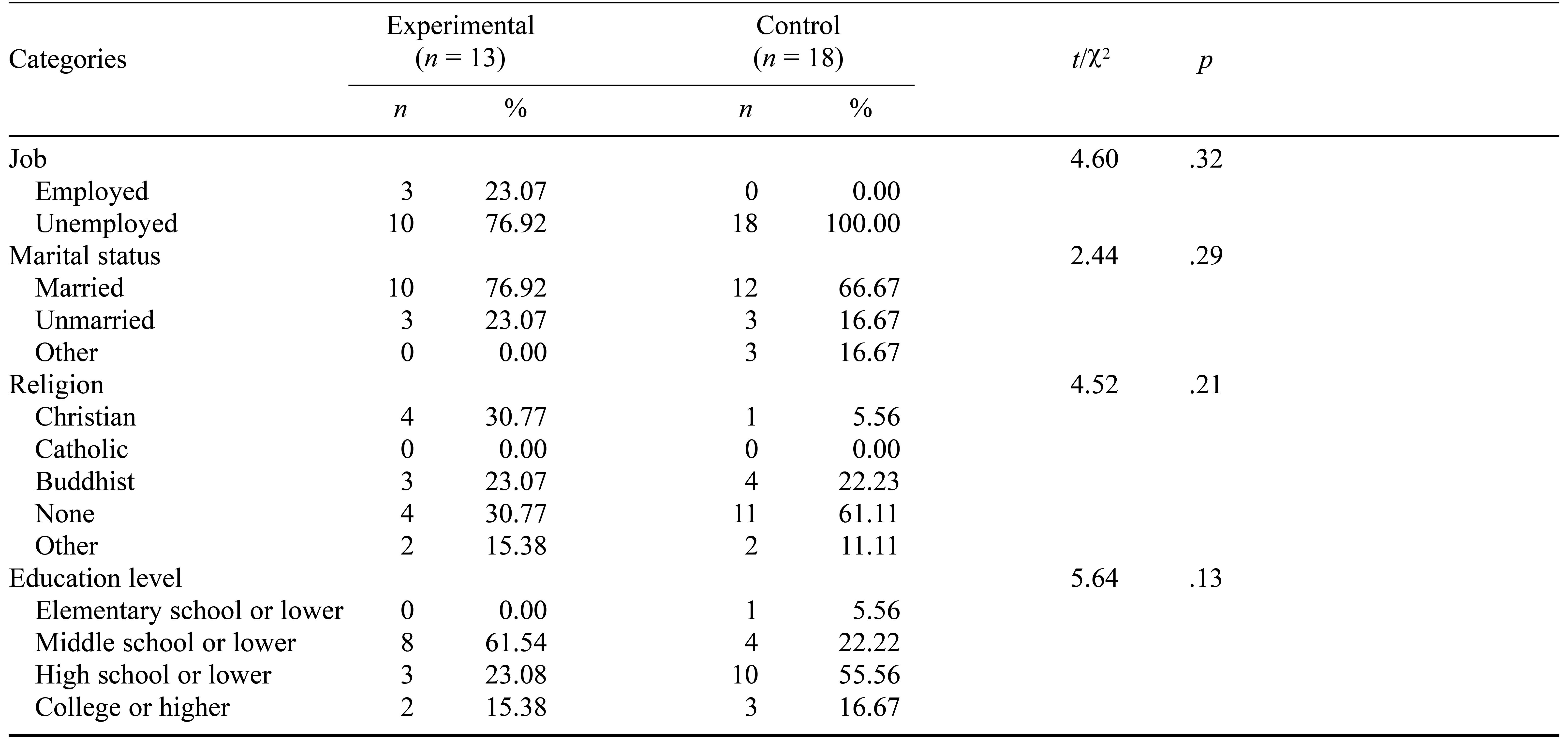
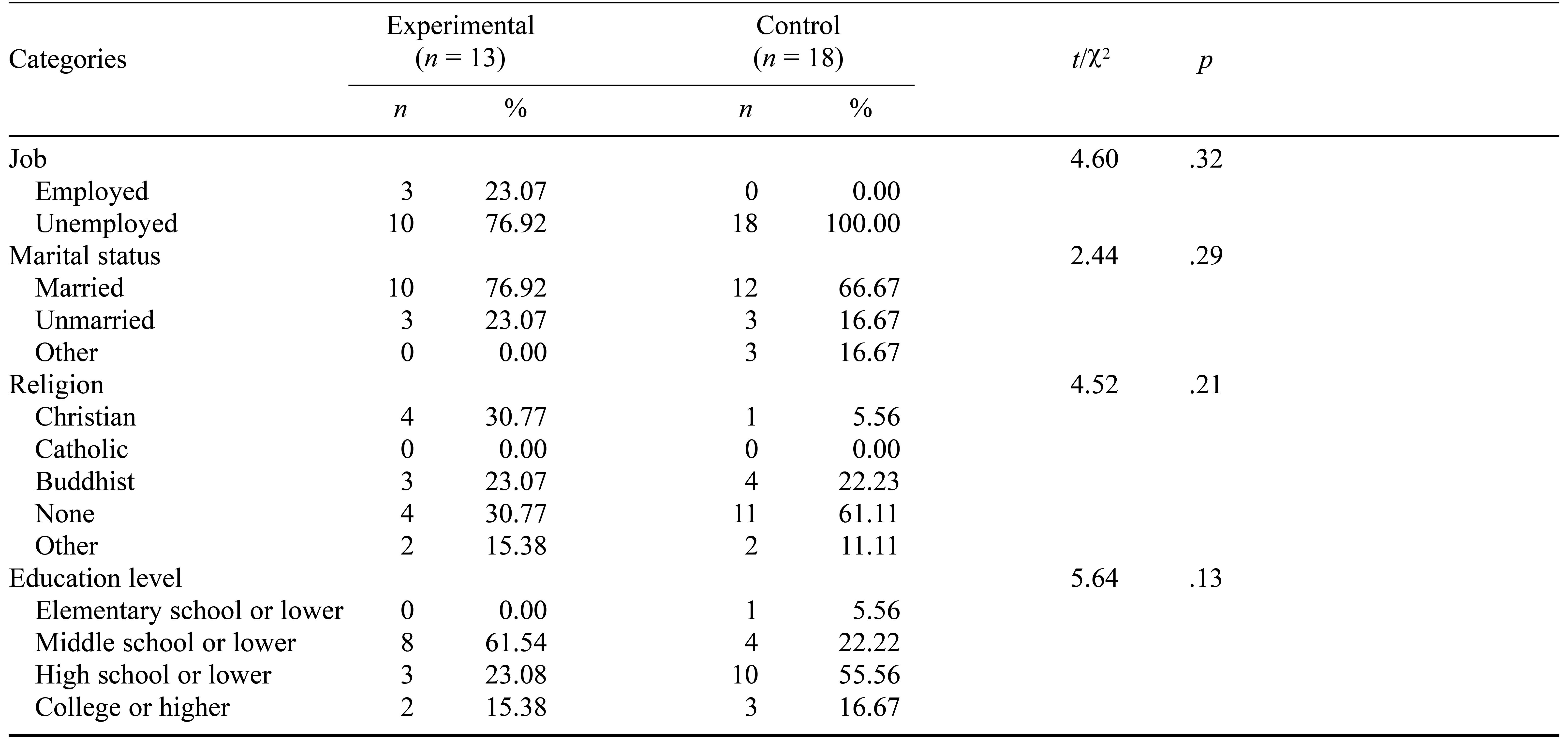
Participants were adults with AUD who had been admitted to psychiatric hospitals in South Korea. We used convenience sampling to select two psychiatric hospitals and invite the rehabilitation program managers to the study. The managers received a detailed explanation regarding the study’s purpose and process. Potential participants were recommended and evaluated with regard to taking part in the study. The inclusion criteria were as follows: (1) diagnosed with AUD, (2) more than 3 days after hospitalization, and (3) being able to participate in all sessions. The exclusion criteria were as follows: (1) expected risk of alcohol delirium tremens, (2) presenting alcohol withdrawal symptoms, and (3) presenting symptoms of cognitive function impairment. To determine the necessary sample size we used the G*Power 3.1 program with a significance level of 0.5, power of 80%, and effect size of 0.5 following Cohen (1988). This revealed that we needed a minimum of 28 participants (14 in each of the experimental and control groups). Considering a 25% dropout rate, we selected and assigned 35 participants, 17 to the experimental group and 18 to the control group. Consequently, through this recruitment process, all the participants were men. In the experimental group the mean age was 55.08 years (SD = 7.75) and in the control group the mean was 50.83 years (SD = 13.58). Participants’ age did not differ by condition (t/χ2 = 1.01, p = .32). Participants’ demographic details are shown in Table 2 in the Results section.
Meditation Training Program
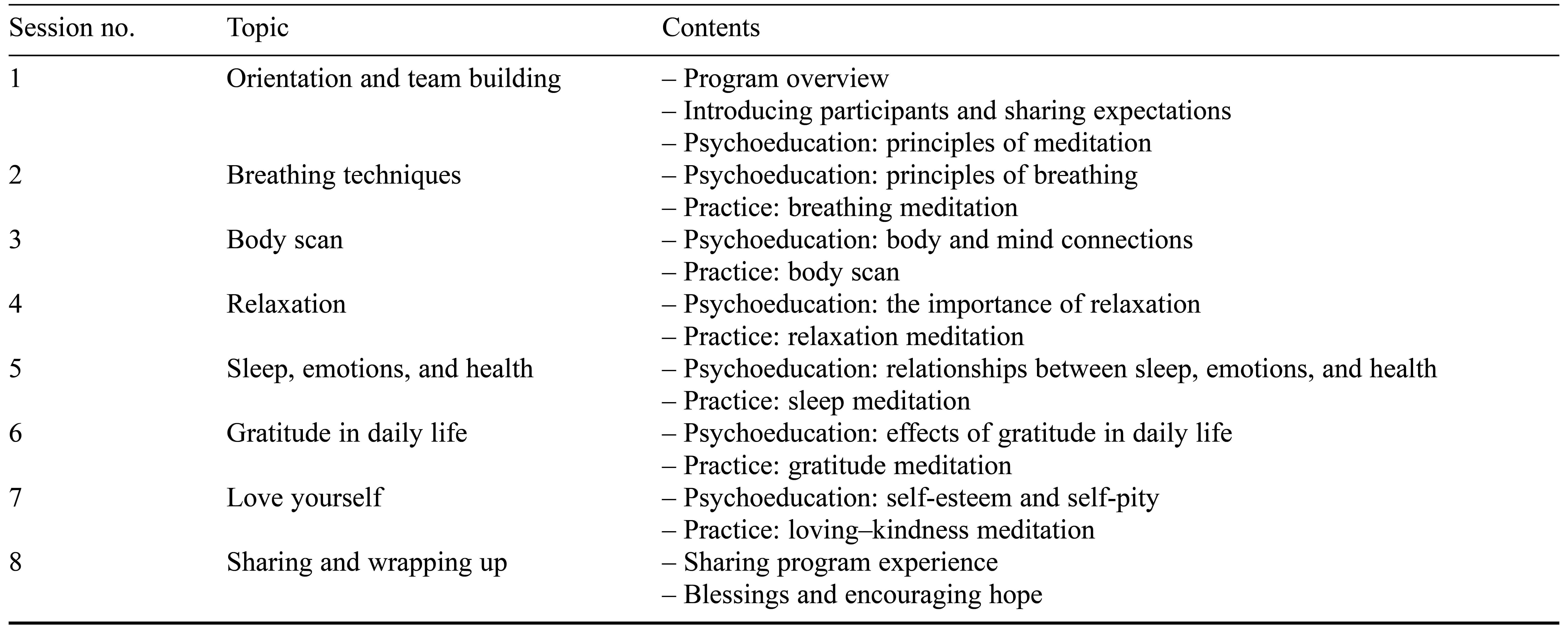
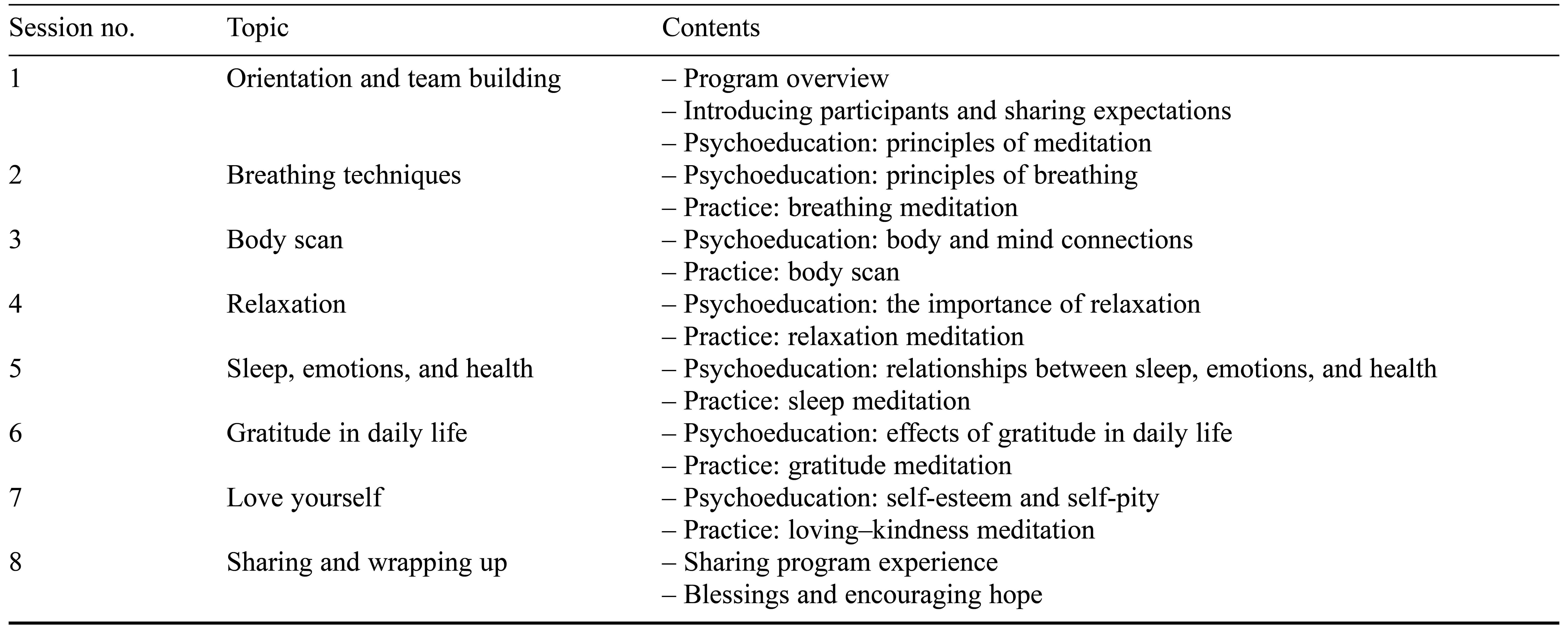
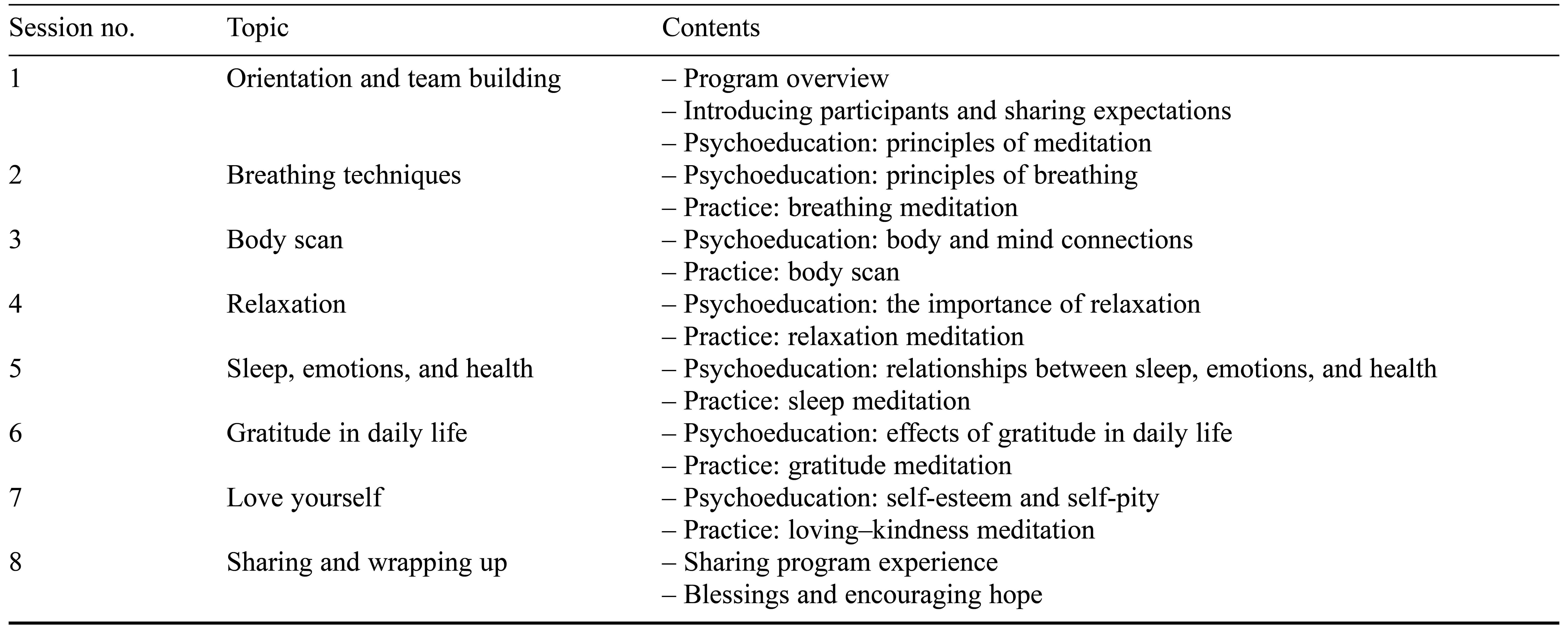
The meditation training program included eight sessions of orientation and team building, body scan, breathing meditation, relaxation meditation, sleep meditation, gratitude meditation, loving–kindness meditation, and psychoeducation (see Table 1). The program was provided for 50 minutes once a week for 8 weeks and was conducted as a group activity led by two mental health nurses who each had more than 5 years’ experience in psychological trauma and mental health nursing.
Table 1. The Meditation Training Program
Data Collection
We collected the data between May 3 and July 18, 2022. We conducted the pretests after receiving the written consent of the participants and post-tests 8 weeks later, when the eighth session of the program was completed. Four clients were dropped from the experimental group because they were discharged before the end of the program. Thus, we analyzed data collected from 13 clients in the experimental group and 18 clients in the control group.
Measures
Mood States
To measure the participants’ mood states, we used the Korean version of the Profile of Mood States-Brief, which was originally developed by McNair et al. (1992). E. J. Kim (2001) translated the scale into Korean and verified its reliability and validity with a sample of 405 Korean students aged 14–30 years. The scale includes 30 items composed of six subcategories: (1) vigor/vitality (“active,” “cheerful”), (2) tension/anxiety (“on edge,” “panicky”), (3) depression/discouraged (“sad,” “unworthy”), (4) anger/hostile (“grouchy,” “annoyed”), (5) fatigue/powerlessness (“worn out,” “sluggish”), and (6) confusion/frustration (“muddled,” “bewildered”). Each item is measured on a 4-point Likert scale ranging from 0 (not at all) to 3 (always). The total mood state value is calculated by subtracting the score for vigor/vitality from the sum of the other scores of the subcategories. The higher the total score, the more negative is the mood state. Cronbach’s alpha in this study was .77, compared to .84 in a previous study with psychiatric patients (Cho & Moon, 2016).
Psychosocial Stress
We utilized the Psychosocial Well-Being Index-Short Form to measure participants’ psychosocial stress. This scale was developed by Chang (2000) and is based on the General Health Questionnaire, which includes 18 items from the original Psychosocial Well-Being Index (Goldberg, 1978). Example items are “I feel very tired and exhausted; even eating is difficult” and “I cannot sleep because of worries.” Each item is measured on a 4-point Likert scale ranging from 0 (always) to 3 (not at all), with a score range of 0–54. The higher the score, the higher the psychosocial stress. Cronbach’s alpha was .86 for this study, compared to .85 in a previous study examining problem drinking and psychosocial stress (Sohn, 2010).
Data Analysis
We analyzed the homogeneity between the experimental and control groups using t tests, chi-square tests, and Fisher’s exact test. We performed a normality check for the dependent variables using the Shapiro–Wilk test. Last, we evaluated the difference in the dependent variables before and after the meditation program for both experimental and control groups using an analysis of covariance (ANCOVA).
Results
Participants’ General Characteristics
Using SPSS 23 software, we calculated the means, frequencies, and standard deviations to describe the participants’ general characteristics (see Table 2). We used t tests, chi-square tests, and Fisher’s exact test to examine the homogeneity between the experimental and control groups. The results showed there were no significant difference in the age (p = .32), marital status (p = .29), religion (p = .21), education level (p = .13), or employment status (p = .32) between the two groups.
Table 2. Participant Characteristics and Homogeneity
Hypothesis Verification
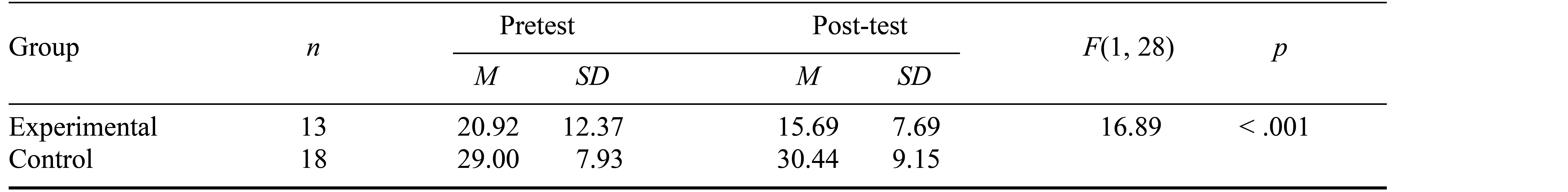
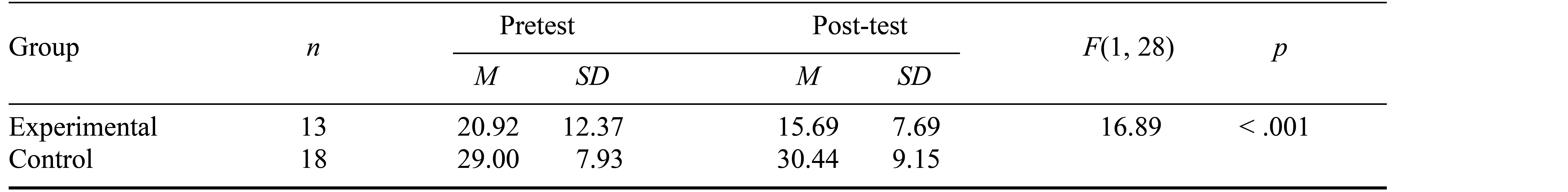
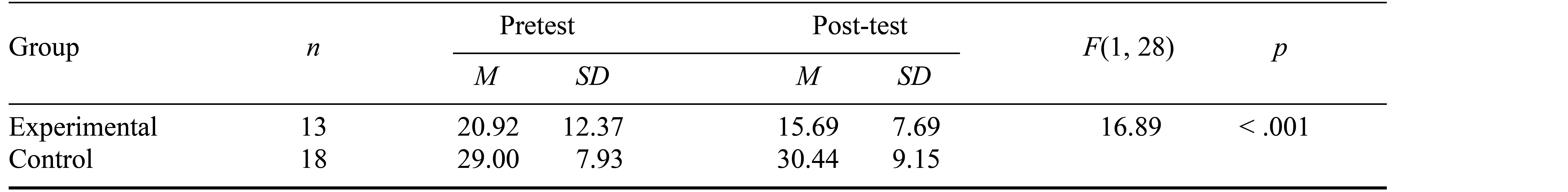
We conducted an ANCOVA by controlling for the prior psychosocial stress score to test the differences in psychosocial stress between the experimental and control groups. The results indicated there was a significant decrease in stress, F(1, 28) = 16.89, p < .001, in the experimental group from 20.92 ± 12.37 points to 15.69 ± 7.69 points, compared to a slight increase in the control group from 29.00 ± 7.93 points to 30.44 ± 9.15 points (see Table 3). Therefore, Hypothesis 1 was supported.
Table 3. Differences Between Groups in Terms of Psychosocial Stress
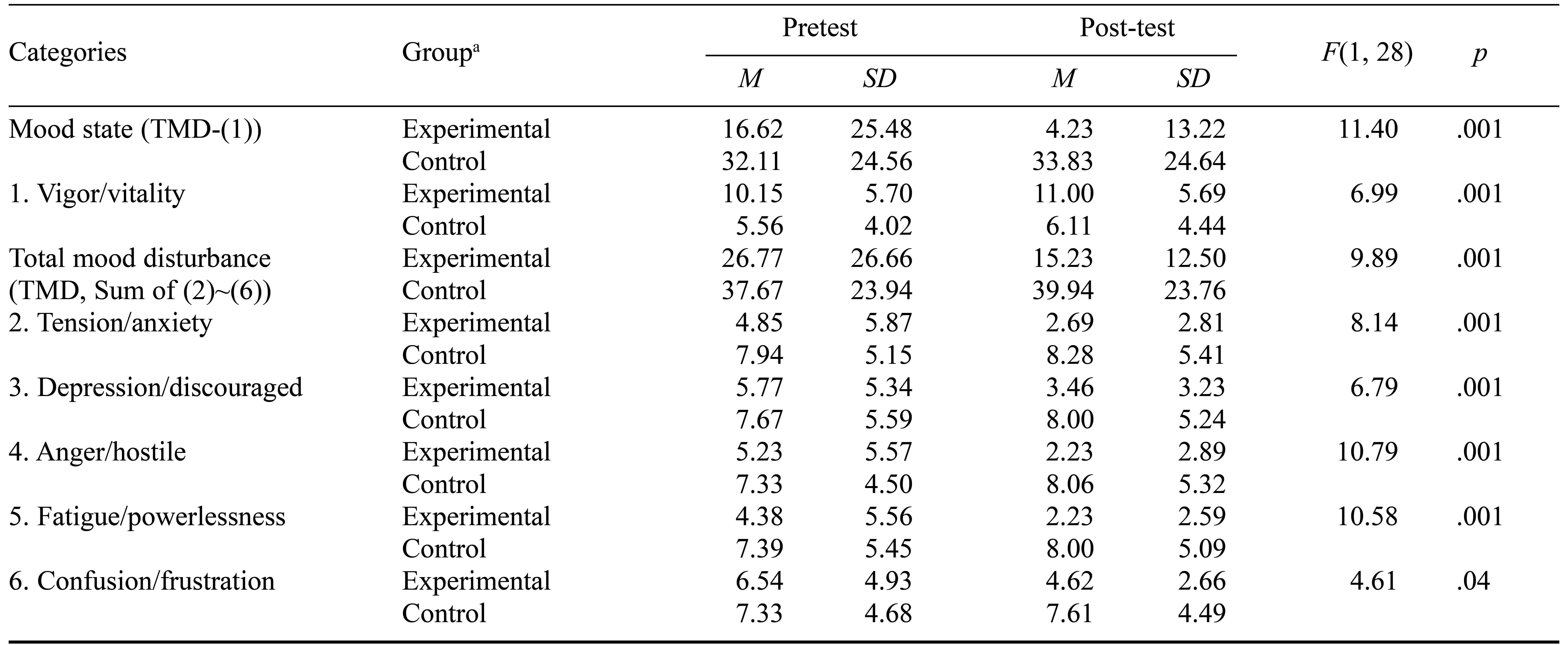
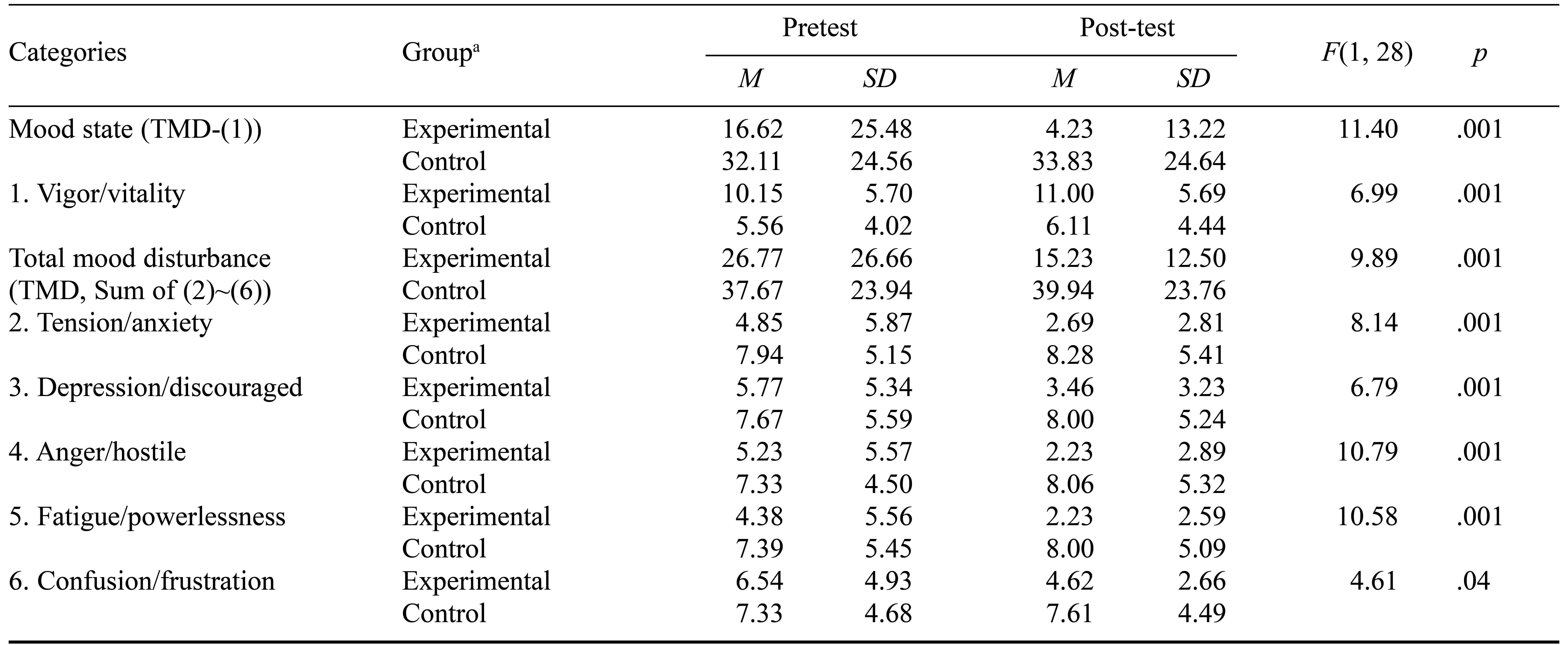
We then conducted an ANCOVA by controlling for the prior mood state score to test the differences in mood states between the experimental and control groups. The results indicated that there was a significant decrease in mood states, F(1, 28) = 11.40, p = .002, in the experimental group from 16.62 ± 25.48 points to 4.23 ± 13.22 points, compared to a slight increase in the control group from 32.11 ± 24.56 points to 33.83 ± 24.64 points. An analysis of the differences in the total mood disturbance scores between the experimental and control groups also demonstrated a significant decrease in the experimental group after the program, F(1, 28) = 9.89, p = .004. In addition, analysis of the differences between the groups’ total mood disturbance subcategories showed significant decreases in the experimental group after the program compared to the control group: tension/anxiety, F(1, 28) = 8.14, p = .008; depression/discouraged, F(1, 28) = 6.79, p = .014; anger/hostile, F(1, 28) = 10.79, p = .003; fatigue/powerlessness, F(1, 28) = 10.58, p = .003; and confusion/frustration, F(1, 28) = 4.61, p = .041. However, vigor/vitality, the positive factor among the mood state subcategories, showed a significant increase in the experimental group after the program compared to the control group, F(1, 28) = 6.99, p = .013 (see Table 4). Consequently, Hypothesis 2 was supported.
Table 4. Differences Between Groups in Terms of Mood State
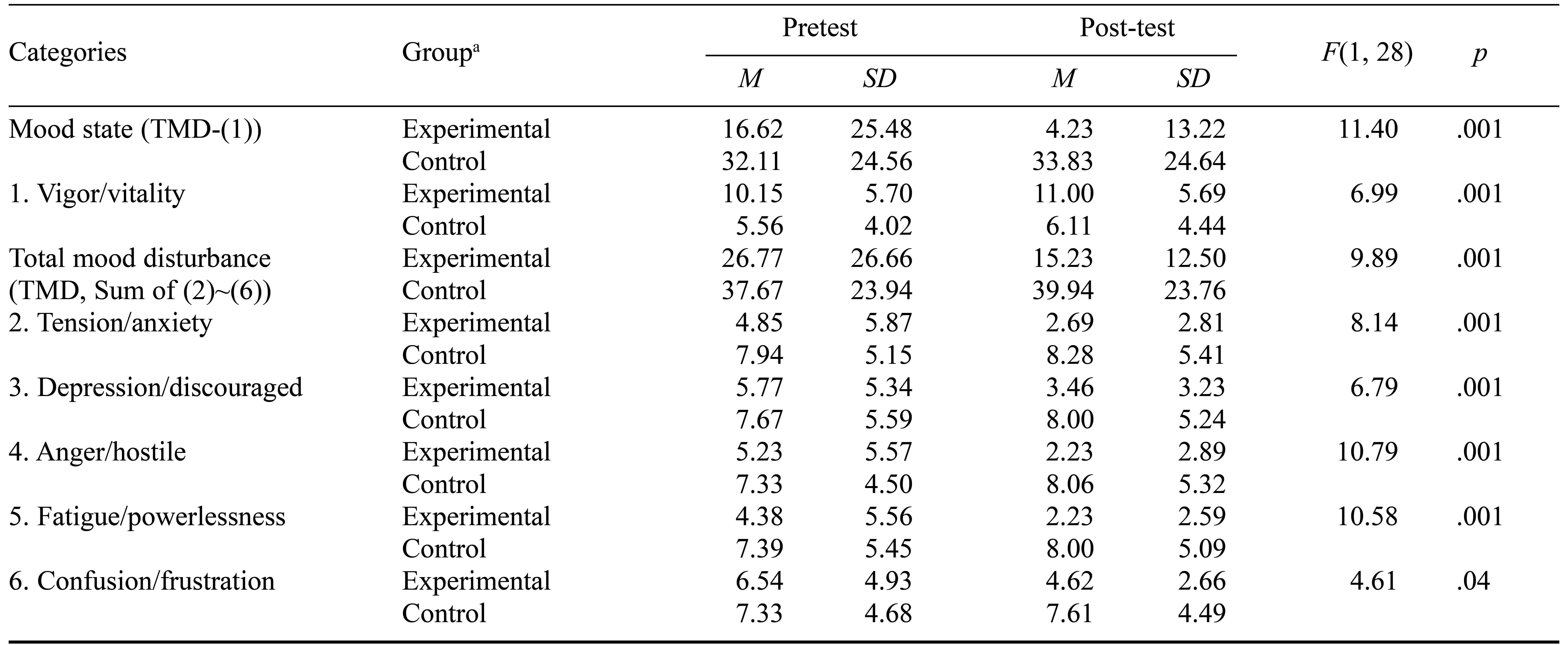
Note. N = 31. a Experimental group n = 13; control group n = 18.
Discussion
In this study inpatient clients with AUD who completed a meditation training program showed a significant decrease in psychosocial stress, supporting Hypothesis 1. This result is in line with a previous study that tested the effect of meditation on perceived stress after eight sessions of meditation and found a significant decrease in the intervention group of clients with AUD versus a slight increase in the control group (K. I. Kang, 2019). In addition, another study on meditation training for clients with AUD revealed an inverse correlation between stress and psychological distress (Gryczynski et al., 2018). These outcomes indicate that meditation training is an efficacious method to lower psychosocial stress in people with AUD.
Furthermore, we found that participants in the meditation training program reported a significant decrease in mood dysregulation, such as depression, anxiety, and anger, compared to the control group, thus supporting Hypothesis 2. These results are consistent with those of a previous study in which the depression, anxiety, and anger scores of people with AUD decreased after an eight-session meditation training course (Shin, 2009). In additional randomized controlled trials on meditation, the depression and anxiety scores of individuals with alcohol dependence also decreased after 8 weeks of meditation training compared to the control group (E. H. Kang, 2014). These results show that meditation training is beneficial for decreasing depression, anxiety, and anger in people with AUD.
Last, the participants in the meditation training program reported a significant decrease in negative emotion and an increase in positive emotion compared to the control group. Therefore, Hypothesis 2 was supported and these results align with those in a previous study that demonstrated a significant decrease in negative emotion and an increase in positive emotion in participants with AUD after completing a 10-week meditation training program (S. H. Park & Lee, 2016). These studies suggest that meditation training can improve mood regulation in clients with AUD.
In summary, this study contributes to nursing knowledge by verifying the efficacy of mood control through a meditation program targeting inpatient clients with AUD. The meditation program presented in this study can be applied to people with AUD in clinical or community mental health contexts. Furthermore, this study can be used to develop and apply intervention programs for people with AUD.
Limitations to this study include the fact that the participants were recruited with convenience sampling and the sample size is small. Thus, caution is required in interpreting or generalizing this study’s results. Further studies are encouraged to include larger samples and use multicenter-based randomized controlled trials.
Conclusion
This study investigated the efficacy of meditation training for psychiatric hospital inpatient clients with AUD in terms of decreasing psychosocial stress and increasing mood regulation. The experimental group that participated in the meditation training program reported a significant decrease in psychosocial stress and negative mood states and an increase in positive mood states compared to the control group. These results demonstrate that meditation training is beneficial in decreasing stress and negative mood states and increasing positive mood states in clients with AUD. More meditation training programs for people with AUD are needed to manage their mood dysregulation, which is one of the most important elements of managing negative mood states.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Baker, T. B., Piper, M. E., McCarthy, D. E., Majeskie, M. R., & Fiore, M. C. (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111(1), 33–51.
Bowen, S., Witkiewitz, K., Clifasefi, S. L., Grow, J., Chawla, N., Hsu, S. H., … Larimer, M. E. (2014). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry, 71(5), 547–556.
Brower, K. J. (2003). Insomnia, alcoholism and relapse. Sleep Medicine Reviews, 7(6), 523–539.
Carey, K. B., & Correia, C. J. (1997). Drinking motives predict alcohol-related problems in college students. Journal of Studies on Alcohol, 58(1), 100–105.
Cavicchioli, M., Movalli, M., & Maffei, C. (2018). The clinical efficacy of mindfulness-based treatments for alcohol and drugs use disorders: A meta-analytic review of randomized and nonrandomized controlled trials. European Addiction Research, 24(3), 137–162.
Chang, S. J. (2000). Standardization of collection and measurement of health statistics data [In Korean]. The Korean Society for Preventive Medicine, Seoul, 2000, 92–143.
Chiesa, A., & Serretti, A. (2014). Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use & Misuse, 49(5), 492–512.
Cho, H., & Moon, J. (2016). The effects of guided imagery activities using music on mood states, and physiological responses of psychiatric inpatients. Rehabilitation Welfare, 20(1), 113–130.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates.
Cooper, M. L., Frone, M. R., Russell, M., & Mudar, P. (1995). Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology, 69(5), 990–1005.
Cox, W. M., & Klinger, E. (1988). A motivational model of alcohol use. Journal of Abnormal Psychology, 97(2), 168–180.
Garland, E. L., Froeliger, B., & Howard, M. O. (2014). Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface. Frontiers in Psychiatry, 4, Article 173.
Garland, E. L., & Howard, M. O. (2018). Mindfulness-based treatment of addiction: Current state of the field and envisioning the next wave of research. Addiction Science & Clinical Practice, 13, Article 14.
Goldberg, D. (1978). Manual of the General Health Questionnaire. NFER Nelson.
Goldstein, R. Z., & Volkow, N. D. (2011). Dysfunction of the prefrontal cortex in addiction: Neuroimaging findings and clinical implications. Nature Reviews Neuroscience, 12, 652–669.
Grant, B. F., Goldstein, R. B., Saha, T. D., Chou, S. P., Jung, J., Zhang, H., … Hasin, D. S. (2015). Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72(8), 757–766.
Gross, J. J. (2013). Handbook of emotion regulation. The Guilford Press.
Gross, J. J. (2014). Handbook of emotion regulation (2nd ed.). The Guilford Press.
Gryczynski, J., Schwartz, R. P., Fishman, M. J., Nordeck, C. D., Grant, J., Nidich, S., … O’Grady, K. (2018). Integration of Transcendental Meditation®TM into alcohol use disorder (AUD) treatment. Journal of Substance Abuse Treatment, 87, 23–30.
Hölzel, B. K., Lazar, S. W., Gard, T., Schuman-Olivier, Z., Vago, D. R., & Ott, U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6(6), 537–559.
Jakubczyk, A., Trucco, E. M., Klimkiewicz, A., Skrzeszewski, J., Suszek, H., Zaorska, J., … Kopera, M. (2020) Association between interoception and emotion regulation in individuals with alcohol use disorder. Frontiers in Psychiatry, 10, Article 1028.
Kang, E. H. (2014). The effects of the meditation program known as MBSR-K on the alcohol abstinence self-efficacy and mental health of people with alcohol dependence (Master’s thesis) [In Korean]. The Catholic University of Korea.
Kang, K. I. (2019). Effects of a mindfulness meditation program for recovering alcoholics (Doctoral dissertation) [In Korean]. Seoul National University.
Khantzian, E. J. (1987). The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. In D. F. Allen (Ed.), The cocaine crisis (pp. 65–74). Springer.
Kim, E. J. (2001). Reliability and validity of the Profile of Mood States–Korean version for use with normal high school and college students (Master’s thesis) [In Korean]. Chungbuk National University.
Kim, S. A., Park, M. W., Seo, J. Y., Kwon, E. J., & Han, H. Y. (2015). Effects of non-pharmacological interventions for alcohol addiction: A meta-analysis [In Korean]. Journal of Korean Society of Nursing Science, 10, Article 518.
Lee, H. K. (2019). Epidemiology of alcohol use disorders and alcohol policy [In Korean]. Journal of Korean Neuropsychiatric Association, 58(3), 152–158.
Li, W., Howard, M. O., Garland, E. L., McGovern, P., & Lazar, M. (2017). Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62–96.
McNair, D. M., Lorr, M., & Droppleman, L. F. (1992). Profile of Mood States manual. Educational and Industrial Testing Service.
Palmer, C. A., Oosterhoff, B., Bower, J. L., Kaplow, J. B., & Alfano, C. A. (2018). Associations among adolescent sleep problems, emotion regulation, and affective disorders: Findings from a nationally representative sample. Journal of Psychiatric Research, 96, 1–8.
Park, H. N., & Yu, S. J. (2005). Effects of meditation training program on self-concept, abstinence self-efficacy, and abstinence in alcoholic patients [In Korean]. Journal of Korean Academy of Psychiatric Mental Health Nursing, 14(3), 304–312.
Park, S. H., & Lee, Y. J. (2016). The effects of mindfulness meditation program on subjective well-being and abstinence self-efficacy of alcohol dependent patients [In Korean]. Korean Journal of Meditation, 6(2), 17–35.
Petit, G., Luminet, O., Maurage, F., Tecco, J., Lechantre, S., Ferauge, M., … de Timary, P. (2015). Emotion regulation in alcohol dependence. Alcohol: Clinical and Experimental Research, 39(12), 2471–2479.
Priddy, S. E., Howard, M. O., Hanley, A. W., Riquino, M. R., Friberg-Felsted, K., & Garland, E. L. (2018). Mindfulness meditation in the treatment of substance use disorders and preventing future relapse: Neurocognitive mechanisms and clinical implications. Substance Abuse and Rehabilitation, 9, 103–114.
Rudebeck, P. H., Bannerman, D. M., & Rushworth, M. F. S. (2008). The contribution of distinct subregions of the ventromedial frontal cortex to emotion, social behavior, and decision making. Cognitive, Affective, & Behavioral Neuroscience, 8, 485–497.
Shin, Y.-C. (2009). Effect of mindfulness-based meditation on negative emotion and self-control of recovering alcohol dependent patients (Master’s thesis) [In Korean]. Chung-Ang University.
Sohn, A.-R. (2010). The effects of stress and depression on problem drinking. Health and Social Science, 27(1), 61–79.
Suzuki, S., Mell, M. M., O’Malley, S. S., Krystal, J. H., Anticevic, A., & Kober, H. (2020). Regulation of craving and negative emotion in alcohol use disorder. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 5(2), 239–250.
Tang, Y.-Y., Hölzel, B. K., & Posner, M. I. (2015). The neuroscience of mindfulness meditation. Nature Reviews Neuroscience, 16, 213–225.
Tang, Y.-Y., Posner, M. I., Rothbart, M. K., & Volkow, N. D. (2015). Circuitry of self-control and its role in reducing addiction. Trends in Cognitive Sciences, 19(8), 439–444.
Tucker, J. A., Chandler, S. D., & Witkiewitz, K. (2020). Epidemiology of recovery from alcohol use disorder. Alcohol Research: Current Reviews, 40(3), 1–12.
World Health Organization. (2018). Global status report on alcohol and health 2018.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Baker, T. B., Piper, M. E., McCarthy, D. E., Majeskie, M. R., & Fiore, M. C. (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111(1), 33–51.
Bowen, S., Witkiewitz, K., Clifasefi, S. L., Grow, J., Chawla, N., Hsu, S. H., … Larimer, M. E. (2014). Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry, 71(5), 547–556.
Brower, K. J. (2003). Insomnia, alcoholism and relapse. Sleep Medicine Reviews, 7(6), 523–539.
Carey, K. B., & Correia, C. J. (1997). Drinking motives predict alcohol-related problems in college students. Journal of Studies on Alcohol, 58(1), 100–105.
Cavicchioli, M., Movalli, M., & Maffei, C. (2018). The clinical efficacy of mindfulness-based treatments for alcohol and drugs use disorders: A meta-analytic review of randomized and nonrandomized controlled trials. European Addiction Research, 24(3), 137–162.
Chang, S. J. (2000). Standardization of collection and measurement of health statistics data [In Korean]. The Korean Society for Preventive Medicine, Seoul, 2000, 92–143.
Chiesa, A., & Serretti, A. (2014). Are mindfulness-based interventions effective for substance use disorders? A systematic review of the evidence. Substance Use & Misuse, 49(5), 492–512.
Cho, H., & Moon, J. (2016). The effects of guided imagery activities using music on mood states, and physiological responses of psychiatric inpatients. Rehabilitation Welfare, 20(1), 113–130.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates.
Cooper, M. L., Frone, M. R., Russell, M., & Mudar, P. (1995). Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality and Social Psychology, 69(5), 990–1005.
Cox, W. M., & Klinger, E. (1988). A motivational model of alcohol use. Journal of Abnormal Psychology, 97(2), 168–180.
Garland, E. L., Froeliger, B., & Howard, M. O. (2014). Mindfulness training targets neurocognitive mechanisms of addiction at the attention-appraisal-emotion interface. Frontiers in Psychiatry, 4, Article 173.
Garland, E. L., & Howard, M. O. (2018). Mindfulness-based treatment of addiction: Current state of the field and envisioning the next wave of research. Addiction Science & Clinical Practice, 13, Article 14.
Goldberg, D. (1978). Manual of the General Health Questionnaire. NFER Nelson.
Goldstein, R. Z., & Volkow, N. D. (2011). Dysfunction of the prefrontal cortex in addiction: Neuroimaging findings and clinical implications. Nature Reviews Neuroscience, 12, 652–669.
Grant, B. F., Goldstein, R. B., Saha, T. D., Chou, S. P., Jung, J., Zhang, H., … Hasin, D. S. (2015). Epidemiology of DSM-5 alcohol use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry, 72(8), 757–766.
Gross, J. J. (2013). Handbook of emotion regulation. The Guilford Press.
Gross, J. J. (2014). Handbook of emotion regulation (2nd ed.). The Guilford Press.
Gryczynski, J., Schwartz, R. P., Fishman, M. J., Nordeck, C. D., Grant, J., Nidich, S., … O’Grady, K. (2018). Integration of Transcendental Meditation®TM into alcohol use disorder (AUD) treatment. Journal of Substance Abuse Treatment, 87, 23–30.
Hölzel, B. K., Lazar, S. W., Gard, T., Schuman-Olivier, Z., Vago, D. R., & Ott, U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6(6), 537–559.
Jakubczyk, A., Trucco, E. M., Klimkiewicz, A., Skrzeszewski, J., Suszek, H., Zaorska, J., … Kopera, M. (2020) Association between interoception and emotion regulation in individuals with alcohol use disorder. Frontiers in Psychiatry, 10, Article 1028.
Kang, E. H. (2014). The effects of the meditation program known as MBSR-K on the alcohol abstinence self-efficacy and mental health of people with alcohol dependence (Master’s thesis) [In Korean]. The Catholic University of Korea.
Kang, K. I. (2019). Effects of a mindfulness meditation program for recovering alcoholics (Doctoral dissertation) [In Korean]. Seoul National University.
Khantzian, E. J. (1987). The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. In D. F. Allen (Ed.), The cocaine crisis (pp. 65–74). Springer.
Kim, E. J. (2001). Reliability and validity of the Profile of Mood States–Korean version for use with normal high school and college students (Master’s thesis) [In Korean]. Chungbuk National University.
Kim, S. A., Park, M. W., Seo, J. Y., Kwon, E. J., & Han, H. Y. (2015). Effects of non-pharmacological interventions for alcohol addiction: A meta-analysis [In Korean]. Journal of Korean Society of Nursing Science, 10, Article 518.
Lee, H. K. (2019). Epidemiology of alcohol use disorders and alcohol policy [In Korean]. Journal of Korean Neuropsychiatric Association, 58(3), 152–158.
Li, W., Howard, M. O., Garland, E. L., McGovern, P., & Lazar, M. (2017). Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62–96.
McNair, D. M., Lorr, M., & Droppleman, L. F. (1992). Profile of Mood States manual. Educational and Industrial Testing Service.
Palmer, C. A., Oosterhoff, B., Bower, J. L., Kaplow, J. B., & Alfano, C. A. (2018). Associations among adolescent sleep problems, emotion regulation, and affective disorders: Findings from a nationally representative sample. Journal of Psychiatric Research, 96, 1–8.
Park, H. N., & Yu, S. J. (2005). Effects of meditation training program on self-concept, abstinence self-efficacy, and abstinence in alcoholic patients [In Korean]. Journal of Korean Academy of Psychiatric Mental Health Nursing, 14(3), 304–312.
Park, S. H., & Lee, Y. J. (2016). The effects of mindfulness meditation program on subjective well-being and abstinence self-efficacy of alcohol dependent patients [In Korean]. Korean Journal of Meditation, 6(2), 17–35.
Petit, G., Luminet, O., Maurage, F., Tecco, J., Lechantre, S., Ferauge, M., … de Timary, P. (2015). Emotion regulation in alcohol dependence. Alcohol: Clinical and Experimental Research, 39(12), 2471–2479.
Priddy, S. E., Howard, M. O., Hanley, A. W., Riquino, M. R., Friberg-Felsted, K., & Garland, E. L. (2018). Mindfulness meditation in the treatment of substance use disorders and preventing future relapse: Neurocognitive mechanisms and clinical implications. Substance Abuse and Rehabilitation, 9, 103–114.
Rudebeck, P. H., Bannerman, D. M., & Rushworth, M. F. S. (2008). The contribution of distinct subregions of the ventromedial frontal cortex to emotion, social behavior, and decision making. Cognitive, Affective, & Behavioral Neuroscience, 8, 485–497.
Shin, Y.-C. (2009). Effect of mindfulness-based meditation on negative emotion and self-control of recovering alcohol dependent patients (Master’s thesis) [In Korean]. Chung-Ang University.
Sohn, A.-R. (2010). The effects of stress and depression on problem drinking. Health and Social Science, 27(1), 61–79.
Suzuki, S., Mell, M. M., O’Malley, S. S., Krystal, J. H., Anticevic, A., & Kober, H. (2020). Regulation of craving and negative emotion in alcohol use disorder. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 5(2), 239–250.
Tang, Y.-Y., Hölzel, B. K., & Posner, M. I. (2015). The neuroscience of mindfulness meditation. Nature Reviews Neuroscience, 16, 213–225.
Tang, Y.-Y., Posner, M. I., Rothbart, M. K., & Volkow, N. D. (2015). Circuitry of self-control and its role in reducing addiction. Trends in Cognitive Sciences, 19(8), 439–444.
Tucker, J. A., Chandler, S. D., & Witkiewitz, K. (2020). Epidemiology of recovery from alcohol use disorder. Alcohol Research: Current Reviews, 40(3), 1–12.
World Health Organization. (2018). Global status report on alcohol and health 2018.