Explicit and implicit attitudes toward people with COVID-19: Need for community mental health services
Main Article Content
During the course of the COVID-19 pandemic, social stigmatization of people who have been infected with the virus has been observed. This study measured the degree of social stigma by examining implicit and explicit attitudes toward people with COVID-19. Explicit attitudes were measured through self-reporting, taking into account the three components of behavior, cognition, and emotion, and we used the Single-Category Implicit Association Test to assess implicit attitudes. The findings show that explicit attitudes toward people with COVID-19 were positive, whereas implicit attitudes trended toward being negative. The results suggest that mental health services and policies are needed to reduce social stigma and prevent the risk of mental health problems among people who have been infected with COVID-19.
With the passage of time, COVID-19 has evolved from an infectious disease into a social problem, with people who have been infected with the virus being stigmatized. Stigma is defined as a negative social attitude attached to the characteristics of an individual that may be regarded as a mental, physical, or social deficiency (Goffman, 1963). Social stigma associated with the COVID-19 stigma began with the label “Chinese Wuhan virus” being assigned on broadcast and social media (Yeh & Tung, 2021); subsequently, the B.1.617.2 strain of the virus, first identified in India, was called the “Indian variant” in the media, prompting an expression of displeasure at this designation by the Indian government (John, 2021).
In general, to simplify their understanding of a changing world, people instinctively classify others into specific social categories (Jhangiani & Tarry, 2014). In high-stress situations, such as the pandemic caused by the worldwide spread of COVID-19, it is easy to identify a target, that is, a person infected with the virus, and classify that individual as belonging to an out-group. Moreover, people possess an in-group bias, preferring this group to members of the out-group (Banaji et al., 2007). The predominance of the in-group is further strengthened when its attributes are evaluated through the belief in a just world hypothesis (Furnham, 2003), in which it is posited that the stronger is one’s belief in a fair world, the easier it is to attribute the difficulties or harm that minority groups experience to their own wrongdoing or personal characteristics. In other words, people who believe strongly in a just world are more likely to think that infection with COVID-19 occurs because of negligence or carelessness. Further, previous studies on scapegoat theory (Richardson & Manglos, 2013; Rothschild et al., 2012) have shown that prejudice and stigma provide an outlet for feelings of anger by transferring the blame for mishaps onto others. This process of transfer indicates that when the public’s feelings of frustration transform into anger and aggression, people infected with COVID-19 may become the target of these negative emotions.
Stigmatization is seen not only in the context of COVID-19, but also in attitudes toward people with various health conditions, including tuberculosis, cancer, human immunodeficiency virus/acquired immunodeficiency syndrome, and obesity (Barrett & Brown, 2008; Chang & Cataldo, 2014; Hatzenbuehler et al., 2013; Van Brakel, 2006). Thus, experiencing social stigma can cause damage to the targeted individual in addition to the negative symptoms of related diseases, and can create mental health problems. According to Kang et al. (2021), COVID-19-related stigma significantly contributes to the risk of depression and posttraumatic stress disorder in people who have been infected with the virus. Lohiniva et al. (2021) reported that people isolated when infected with COVID-19 experienced fear and anxiety because social stigma led to difficulties in interacting with others even after their isolation period was complete.
Stigma can be explored from various angles by analyzing attitudes. According to Vaughan and Hogg (2005), an attitude is a relatively enduring organization of beliefs, feelings, and behavioral tendencies toward socially significant objects, groups, events, or symbols. Attitudes consist of three components (Ajzen, 1993; Allport, 1954): The affective component involves a person’s feelings/emotions about an object, the behavioral component relates to behavioral reactions toward the object, and the cognitive component refers to beliefs and knowledge about the object.
Attitudes toward a specific object can be further divided into two subcategories: explicit and implicit. Explicit attitudes are conscious, expressed directly, and can be easily reported; thus, they are usually measured through self-reported tests. In contrast, implicit attitudes are based on automated processing, are not expressed openly, and are difficult to control consciously (Bang et al., 2010); therefore, the Implicit Association Test (IAT; Greenwald et al., 2003) is a common method of assessment. Explicit and implicit attitudes toward the same object may coincide or differ. Discrepancy between the two attitude types is observed more often when socially sensitive issues, such as prejudice against age, gender, and racial categories, are targeted (Greenwald et al., 2002; Tam et al., 2006). Absent or weak implicit–explicit relationships show that these psychological constructs are related yet distinctly different. An implicit attitude that is difficult to control is considered more authentic than an explicit attitude that can be cognitively restrained (Greenwald et al., 1998; Nosek, 2007; Nosek & Smyth, 2007). A negative implicit attitude can be expressed as an implicit bias when it becomes evident in different domains of society, resulting in the enduring stereotypification of specific objects (Charlesworth & Banaji, 2019). A feeling or bias that is implicitly present but not explicitly revealed may be more difficult to counter or prevent. Therefore, public attitudes toward persons with COVID-19 must be examined to prevent progression from stigma to long-term discrimination.
The purpose of this study was to examine implicit and explicit attitudes toward people with COVID-19, and to explore associated social stigma by revealing the relationship between implicit and explicit attitudes in this context. Our main research questions were as follows:
Research Question 1: What is the level of the participants’ explicit and implicit attitudes toward persons with COVID-19?
Research Question 2: Is there a relationship between explicit and implicit attitudes toward persons with COVID-19?
Method
Participants
Research information posting, recruitment, and data collection were conducted from November 3, 2020, to March 7, 2021, targeting students who were enrolled at a university in South Korea. Because respondents must use their fingers when completing the Single-Category Implicit Association Test, students who had pain or difficulty in using their fingers were excluded from participating in the study. In addition, in the case of students who had contracted COVID-19 prior to the time of this research, there was a possibility of in-grouping with the hypothetical group described in the study scenario as having had COVID-19, so we recruited as participants only those who had never been infected with COVID-19, who could be classified as an out-group. To control for the effect of participants’ demographic characteristics on the results, we set an age range of between 20 and 29 years, and men and women were represented equally. After one respondent’s data were deemed unusable, the final sample comprised 30 men and 30 women (Mage = 23.62 years, SD = 3.87).
Procedure
This study was conducted with the approval of the Institutional Review Board of Chung-Ang University, and all respondents provided informed consent to participate in the study. After seeking and receiving online applications to take part in the research, we contacted the applicants directly to inform them about the purpose and content of the study, and set up the implementation schedule. The investigation was conducted in a laboratory on a scheduled day. After hearing the explanation of the purpose of the study, the students filled out the consent form. Participants completed the Single-Category Implicit Association Test (SC-IAT) task (see “Measures” subsection below) individually, coming to the laboratory one at a time at a prearranged time. All participants used the same computer in the laboratory, and the test took about 30 minutes to complete. Next, they filled out a self-report survey and provided personal information. Survey data were collected thereafter. Anonymized analysis was conducted to protect the respondents’ personal information.
Measures
Implicit Attitude Toward People With COVID-19
This study used the SC-IAT to determine implicit attitudes toward people with COVID-19. The Inquisit 5.0 program was used to present the SC-IAT, in which the syntax developed by Karpinski and Steinman (2006) was modified to reflect our focal variables.
Stimuli Selection Procedure for Single-Category Implicit Association Test
We first selected photographic stimuli. Using the phrase “COVID-19 confirmed persons” as the keywords on Naver and Google, which are the Korean public’s most preferred Internet portal service providers (Internet Trend, 2020), we randomly extracted 18 representative images. The validity of the search was then established through a screening test with 41 students (17 men, 24 women; Mage = 24.66 years, SD = 2.31) recruited from a university in Seoul. The participants were instructed to indicate how well the images represented persons confirmed as being infected with COVID-19, on a scale from 1 = not at all to 10 = completely. Subsequently, we selected six stimulus photographs with scores of eight points and above (M = 8.45, SD = 0.36). Figure 1 shows examples of these photographs. We translated four positive words (safe, reliable, responsible, and sane) and four negative words (dangerous, unpredictable, crazy, and insane) used by Schreger and Kimble (2017) for use as stimuli in our study.

Figure 1. Sample Stimulus Photographs
Note. The text in the sign in the photograph on the right says “Do not enter. Confirmed case of COVID-19 on this site.”
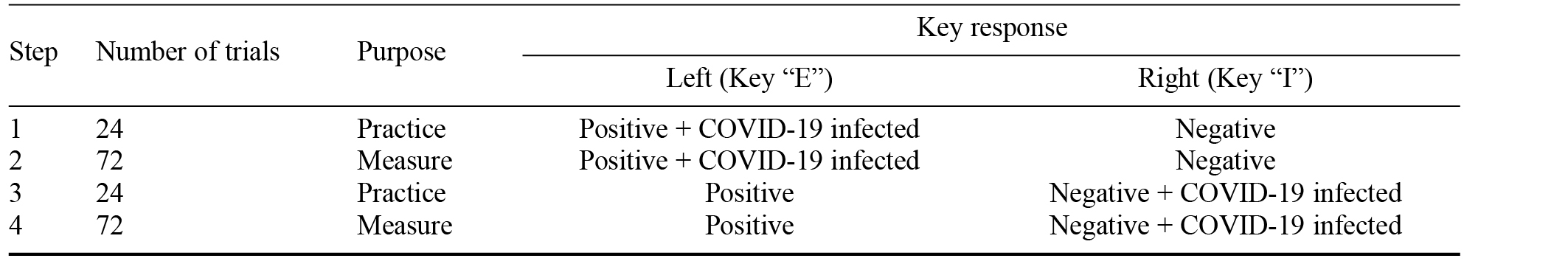
Structure of the Single-Category Implicit Association Test
The steps in completing the SC-IAT are set out in Table 1. The first stage consisted of 24 cycles used as practice trials, in which the target category of people with COVID-19 and positive words were classified through the same response key. The second step was the same as the first, but was an actual measurement step consisting of 72 cycles. Step three was executed by changing the target category name presented at the top of the screen for 24 practice trials, so that people with COVID-19 and the negative words shared the same reaction key, then Step 4 involved another measurement round of 72 cycles. In all trials the target stimulus was displayed on screen until either the participant responded or 1,500 ms had elapsed.
Table 1. Single-Category Implicit Association Test Steps to Measure Implicit Attitude Toward People With COVID-19
The implicit attitude toward people with COVID-19 can be measured by the difference between the average response delay time, when the target category is paired with a positive word and a negative word through the SC-IAT. The adjusted difference values were converted to the same 7-point Likert scale we used to measure explicit attitudes, following the standard procedure suggested by Karpinski and Steinman (2006). This approach facilitated comparison between the two dependent variables (see Table 2).
Table 2. Criteria for the Converted Adjusted Difference Values to Measure Implicit Attitude Toward People With COVID-19
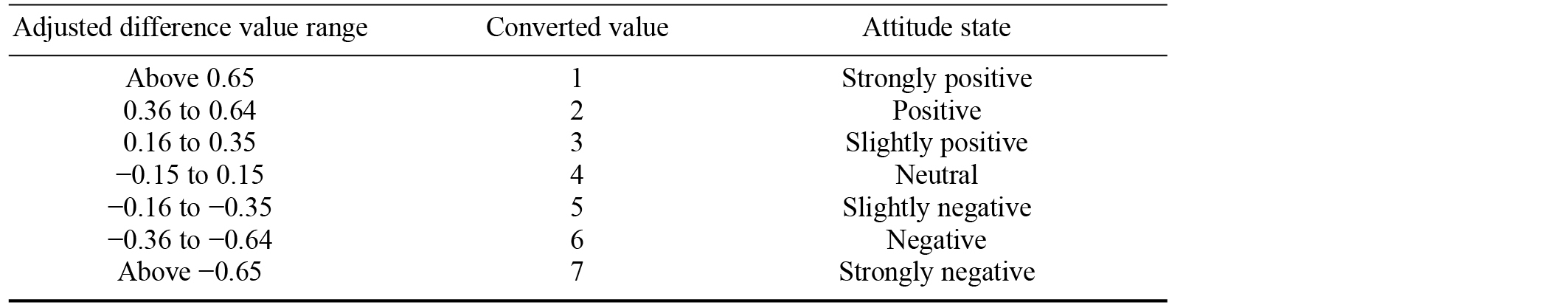
Note. A lower value indicates a positive attitude and a higher value indicates a negative attitude.
Explicit Attitude Toward People With COVID-19
We modified the measures used by Kim (2002) to assess the three components of explicit attitudes: behavioral, cognitive, and emotional. The behavioral component was measured with seven items to assess social distance (score range = 7–49), such as “I would not mind getting acquainted with someone who has previously been infected with COVID-19”; the cognitive component was measured with three items to assess negative stereotypes (score range = 3–21), such as “People who have been infected with COVID-19 harm others”; and the emotional component was measured with three items to assess negative emotions (score range = 3–21), such as “I do not like people who have COVID-19.” Each component was measured on a 7-point Likert scale ranging from 1 = strongly agree to 7 = strongly disagree; therefore, the higher the score, the more negative was the explicit attitude toward people with COVID-19. We used reverse-scoring to make the comparison with SC-IAT scores. Cronbach’s alpha in this study was .93.
Data Analysis
Study data were processed using SPSS 26.0. Internal consistency reliability was analyzed by calculating Cronbach’s alpha values. Further, we performed descriptive statistical analyses of participants’ demographic characteristics and their explicit and implicit attitudes toward people with COVID-19. To compare the scores for explicit and implicit attitudes, we calculated the average values by converting attitude differences scores. Thereafter, the relationship between the participants’ implicit and explicit attitudes was examined through Pearson correlation analysis to confirm possible discrepancies in the two types.
Results
Participants’ Demographic Characteristics
Table 3 shows the participants’ demographic characteristics.
Table 3. Demographic Characteristics of the Participants
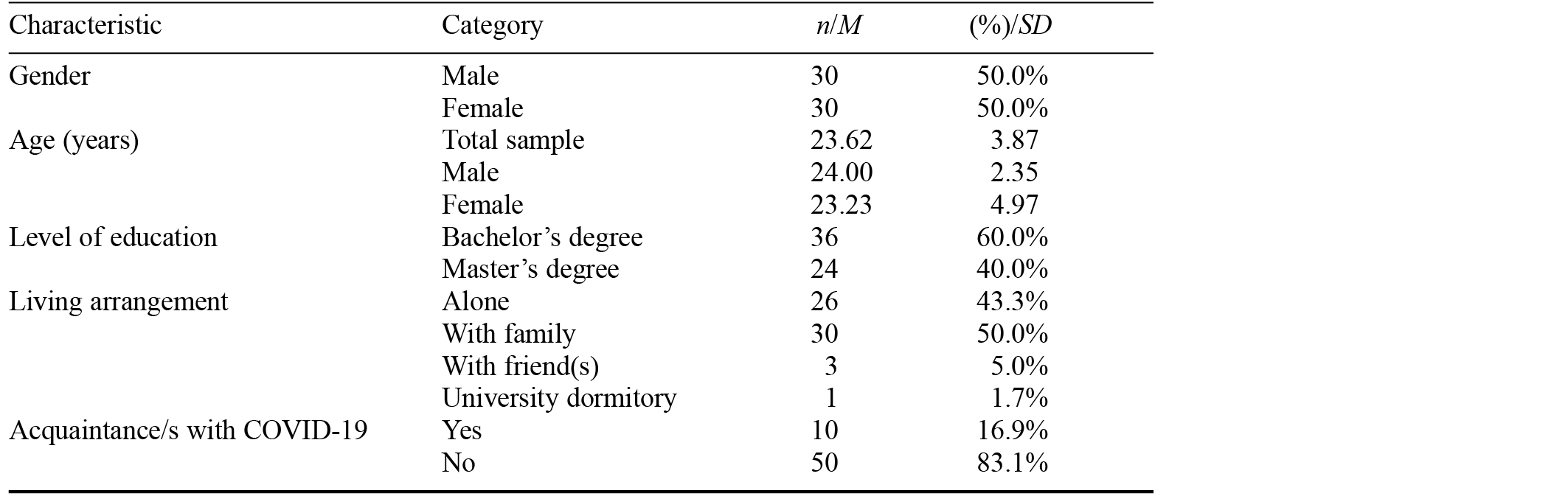
Note. N = 60.
Participants’ Implicit and Explicit Attitudes Toward People With COVID-19
Figure 2 shows a comparison of the percentage of responses for the two attitude types and each of the three explicit attitude components toward people with COVID-19. We found it noteworthy that there was no negative trend overall for the cognitive component of explicit attitude; however, 52.6% of responses in the implicit attitude test were negative.
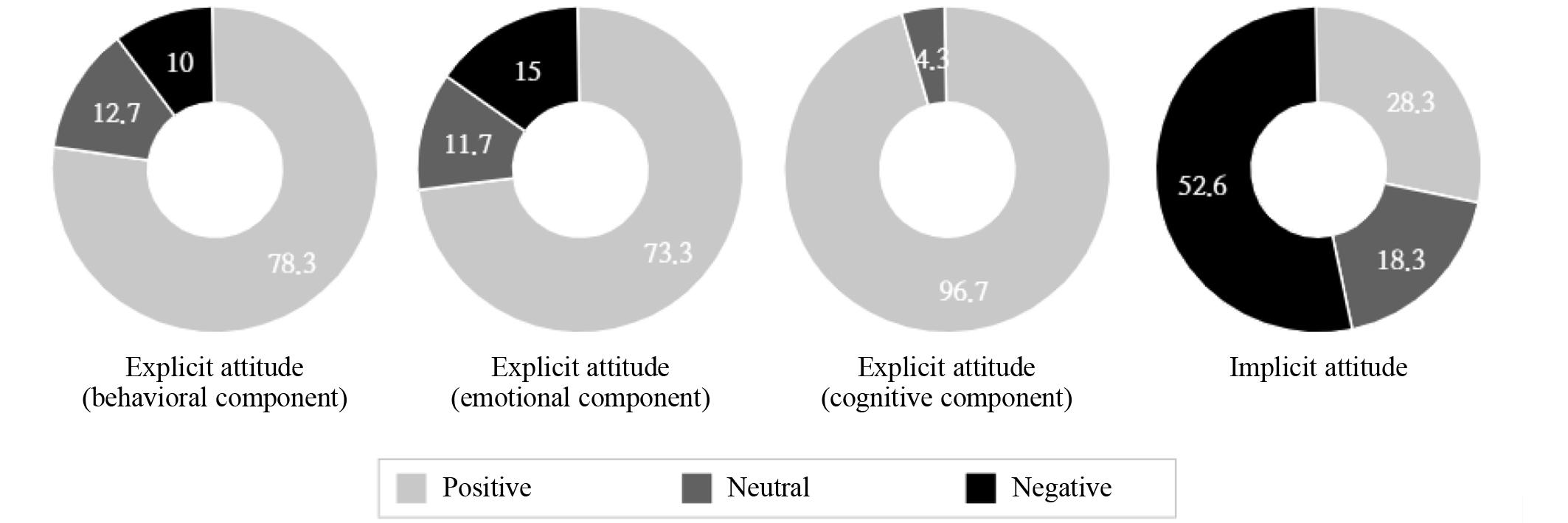
Figure 2. Percentage Comparison of Implicit and Explicit Attitudes Toward People With COVID-19
Note. N = 60. On the 7-point Likert scale, positive = score of 1–3 points for an item; neutral = score of 4 points; negative = score of 5–7 points.
Table 4 shows the average scores for implicit and explicit attitudes toward people with COVID-19. The average score for implicit attitude was 4.42 (± 1.63). This value lies in the slightly negative attitude state range (possible range = 1–7; 4 points indicates a neutral state). Among the explicit attitude components, the behavioral component averaged a score of 2.60 (± 1.32), the emotional component average was a score of 2.58 (± 1.53), and the cognitive component averaged 1.72 (± 0.80); thus, all can be categorized as fitting the positive state.
Table 4. Correlation of Explicit and Implicit Attitudes Toward People With COVID-19
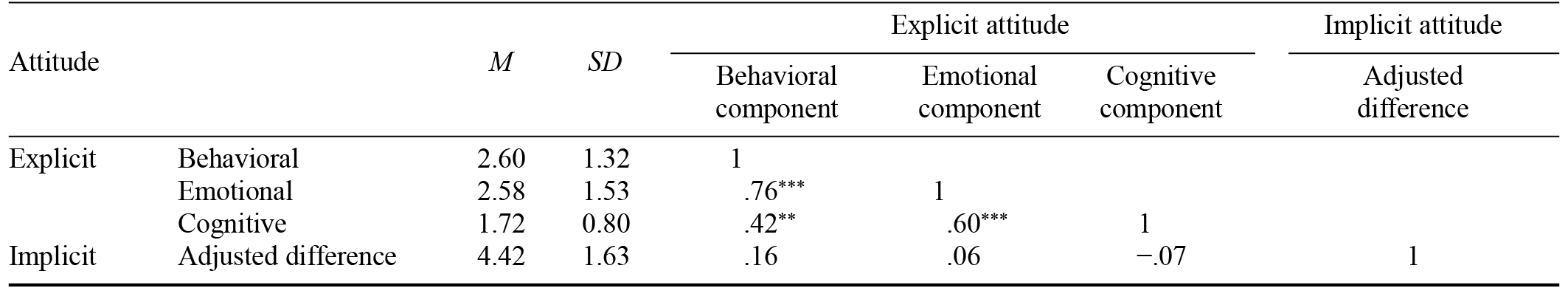
Note. * p < .05. ** p < .01. *** p < .001.
Relationship Between Implicit and Explicit Attitudes Toward People With COVID-19
For a multifaceted analysis of attitudes toward people with COVID-19, we measured explicit attitude by classifying the three characteristics of attitude. These characteristics were measured through a self-report test; thus, it was possible that the components would be highly correlated, which is what we found. However, we found no significant correlation between implicit attitude scores and scores on all the constituent attributes of explicit attitude. This suggests the possibility of discrepancies in people’s attitudes, such that they may outwardly have a positive or neutral attitude toward people with COVID-19, but implicitly maintain a negative attitude.
Discussion
COVID-19 poses grave physical and mental health risks to people worldwide. Because the virus is transmitted through contact with others, infected persons can be stigmatized, as has been historically experienced by people affected by various other infectious diseases. In this study we measured explicit and implicit attitudes of the general public toward people with COVID-19, and found that inconsistency between these two attitude types could explain the social stigma that is rising against people who have been infected with the virus. As expected, explicit attitudes were positive, especially in regard to the cognitive component. In contrast, implicit attitudes trended toward being negative, and our correlation results revealed a discrepancy between implicit and explicit attitudes.
Theoretical and Practical Implications
Our participants displayed a positive explicit attitude toward people with COVID-19, especially in regard to the cognitive component of attitude, which is easier for the individual to control than the behavioral or emotional components. Because explicit attitudes are influenced by social desirability, in the context of research, these attitudes are more likely than are implicit attitudes to elicit socially exemplary answers. However, our finding of a negative implicit attitude is also significant, even though it was not strongly negative.
Additionally, our correlation results revealed a discrepancy between implicit and explicit attitudes toward the same object, that is, people with COVID-19. In line with previous studies, this suggests that people with COVID-19 are socially sensitive subjects. Jordan et al. (2012) suggested that variance between implicit and explicit attitudes causes mental discomfort, creating psychological defenses that ultimately lead to discrimination. Rudman and Ashmore (2007) found that implicit attitudes and beliefs create intergroup discrimination above and beyond their explicit attitudinal and belief counterparts. Therefore, the two types of attitude toward people with COVID-19 will eventually lead to discrimination against this group.
As has been pointed out in previous studies related to other infectious diseases, discrimination and social exclusion can undermine efforts to identify, isolate, and contain the transmission of a virus. Social stigma reduces the likelihood of people who have been infected coming forward for appropriate medical help (Bonadonna et al., 2017). They may also take extreme actions, such as attempting to escape during quarantine and/or hospitalization (Des Jarlais et al., 2006; Parker & Aggleton, 2003). Such uncontrollable actions endanger society as a whole.
As a consequence, efforts are needed to reduce social stigma. Van Brakel (2006) suggested examining stigma from various perspectives, and stated that this would be helpful in reducing the stigma; including monitoring and evaluation of the impact of interventions to reduce stigma in the community, examining and comparing the efficacy of different strategies and interventions, and evaluating the cost effectiveness of various interventions to reduce stigma or to mitigate the impact of stigma. By providing data on stigma for advocacy work, the case of people involved in advocacy on behalf of those stigmatized would be strengthened. Such data would awaken the interest of the public to the plight of those affected by the stigma. According to Heijnders and Van Der Meij (2006), community-centered interventions are more effective in reducing stigma than are individual interventions. Besides, in the case of COVID-19, it has been found that a lack of knowledge of the virus is a determinant of the discrimination level against people who have been infected (Liu et al., 2021). More research is needed to find the most effective ways to prevent social stigma, with consideration given to the results of these studies.
Limitations and Directions for Future Research
This study has some limitations. We recruited a small sample by controlling for participants’ gender and age. Therefore, further research will be needed to generalize our results to a sample of a more diverse population. Another possible limitation is that we presented all participants with the SC-IAT before the measure of explicit attitudes. As the implicit attitude has less effect on cognitive control than the explicit attitude does, the implicit attitude is generally measured first when measuring the two together. Thus, we followed this practice. To expand the scope of our research, attitudes could be analyzed or explored through more diverse sociocultural variables. Additionally, because attitudes toward people with COVID-19 may change depending on the progression of the virus, it is necessary to continue to analyze the trend through longitudinal studies, as opposed to employing an experimental design with a single time point, which we used.
Conclusion
In this study we performed a multifaceted analysis through objective and diverse investigation methods of how people who have been infected with COVID-19 are viewed. We confirmed the inconsistency of participants’ explicitly positive and implicitly negative attitudes toward people with COVID-19. Similar results have been obtained when measuring attitudes toward sensitive issues like social prejudice, suggesting that people who have been infected with the virus are targets of social stigmatization in this pandemic. In addition, this study is meaningful because we objectively measured and analyzed attitudes toward people with COVID-19, beyond the examination of self-reports on the stigma experienced by this group. Our results demonstrate the need to develop social intervention policies and strategies to respond effectively and reduce social stigma and negative attitudes displayed toward patients confirmed as having COVID-19 in the current pandemic. As it is more effective to address social stigma at the societal level than at an individual-only level, there is a need for continued social and public research on attitudes toward people with COVID-19 and related factors.
References
Ajzen, I. (1993). Attitude theory and the attitude-behavior relation. In D. Krebs & P. Schmidt (Eds.), New directions in attitude measurement (pp. 41–57). Walter de Gruyter.
Allport, G. W. (1954). The historical background of modern social psychology. In G. Lindzay (Ed.), Handbook of social psychology (pp. 3–56). Addison Wesley.
Banaji, M. R., Baron, A. S., Dunham, Y., & Olson, K. (2007). The development of intergroup social cognition: Early emergence, implicit nature, and sensitivity to group status. In M. Killen & S. Levy (Eds.), Intergroup attitudes and relations in childhood through adulthood (pp. 87–102). Oxford University Press.
Bang, H. J., Noh, K. R., & Jung, S. J. (2010). The development of implicit and explicit race attitudes in Korean in the multi-cultural age [In Korean]. The Korean Journal of Developmental Psychology, 23(2), 125–140. https://bit.ly/3jtdLqU
Barrett, R., & Brown, P. J. (2008). Stigma in the time of influenza: Social and institutional responses to pandemic emergencies. The Journal of Infectious Diseases, 197(1), 34–37.
https://doi.org/10.1086/524986
Bonadonna, L. V., Saunders, M. J., Zegarra, R., Evans, C., Alegria-Flores, K., & Guio, H. (2017). Why wait? The social determinants underlying tuberculosis diagnostic delay. PLoS ONE, 12(9), Article e0185018.
https://doi.org/10.1371/journal.pone.0185018
Chang, S.-H., & Cataldo, J. K. (2014). A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma. The International Journal of Tuberculosis and Lung Disease, 18(2), 168–173.
https://doi.org/10.5588/ijtld.13.0181
Charlesworth, T. E. S., & Banaji, M. R. (2019). Patterns of implicit and explicit attitude: I. Long-term change and stability from 2007 to 2016. Psychological Science, 30(2), 174–192.
https://doi.org/10.1177/0956797618813087
Des Jarlais, D. C., Galea, S., Tracy, M., Tross, S., & Vlahov, D. (2006). Stigmatization of newly emerging infectious diseases: AIDS and SARS. American Journal of Public Health, 96(3), 561–567.
https://doi.org/10.2105/AJPH.2004.054742
Furnham, A. (2003). Belief in a just world: Research progress over the past decade. Personality and Individual Differences, 34(5), 795–817.
https://doi.org/10.1016/S0191-8869(02)00072-7
Goffman, E. (1963). Stigma: Notes on the management of spoiled identity. Prentice Hall.
Greenwald, A. G., Banaji, M. R., Rudman, L. A., Farnham, S. D., Nosek, B. A., & Mellott, D. S. (2002). A unified theory of implicit attitudes, stereotypes, self-esteem, and self-concept. Psychological Review, 109(1), 3–25.
https://doi.org/10.1037/0033-295X.109.1.3
Greenwald, A. G., McGhee, D. E., & Schwartz, J. L. K. (1998). Measuring individual differences in implicit cognition: The Implicit Association Test. Journal of Personality and Social Psychology, 74(6), 1464–1480.
https://doi.org/10.1037//0022-3514.74.6.1464
Greenwald, A. G., Nosek, B. A., & Banaji, M. R. (2003). Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology, 85(2), 197–216.
https://doi.org/10.1037/0022-3514.85.2.197
Hatzenbuehler, M. L., Phelan, J. C., & Link, B. G. (2013). Stigma as a fundamental cause of population health inequalities. American Journal of Public Health, 103(5), 813–821.
https://doi.org/10.2105/AJPH.2012.301069
Heijnders, M., & Van Der Meij, S. (2006). The fight against stigma: An overview of stigma-reduction strategies and interventions. Psychology, Health & Medicine, 11(3), 353–363.
https://doi.org/10.1080/13548500600595327
Internet Trend. (2020, September 10). Logger [In Korean]. https://bit.ly/3amQ2mX
Jhangiani, R., & Tarry, H. (2014). Principles of social psychology (1st international ed.). https://bit.ly/3jx7xX7
John, T. (2021, June 1). The stigma of variant names. Cable News Network. https://cnn.it/3jxcqzr
Jordan, C. H., Logel, C., Spencer, S. J., & Zanna, M. P. (2012). Discrepancies between implicit and explicit attitudes, prejudices, and self-esteem: A model of simultaneous accessibility. In B. Gawronski & F. Strack (Eds.), Cognitive consistency: A fundamental principle in social cognition (pp. 202–222). Guilford Press.
Kang, E., Lee, S. Y., Kim, M. S., Jung, H., Kim, K. H., Kim, K.-N., … Sohn, J. H. (2021). The psychological burden of COVID-19 stigma: Evaluation of the mental health of isolated mild condition COVID-19 patients. Journal of Korean Medical Science, 36(3), Article e33.
https://doi.org/10.3346/jkms.2021.36.e33
Karpinski, A., & Steinman, R. B. (2006). The Single Category Implicit Association Test as a measure of implicit social cognition. Journal of Personality and Social Psychology, 91(1), 16–32.
https://doi.org/10.1037/0022-3514.91.1.16
Kim, S. H. (2002). Attitude and social distance towards minority groups in Korean society [In Korean]. Korean Journal of Social Issues, 1, 169–206. https://bit.ly/39DoRUo
Liu, R., Nicholas, S., Leng, A., Qian, D., Maitland, E., & Wang, J. (2021). The influencing factors of discrimination against recovered Coronavirus disease 2019 (COVID-19) patients in China: A national study. Human Vaccines & Immunotherapeutics. Advance online publication.
https://doi.org/10.1080/21645515.2021.1913966
Lohiniva, A.-L., Dub, T., Hagberg, L., & Nohynek, H. (2021). Learning about COVID-19-related stigma, quarantine and isolation experiences in Finland. PLoS ONE, 16(4), Article e0247962.
https://doi.org/10.1371/journal.pone.0247962
Nosek, B. A. (2007). Implicit–explicit relations. Current Directions in Psychological Science, 16(2), 65–69.
https://doi.org/10.1111/j.1467-8721.2007.00477.x
Nosek, B. A., & Smyth, F. L. (2007). A multitrait-multimethod validation of the Implicit Association Test. Experimental Psychology, 54(1), 14–29.
https://doi.org/10.1027/1618-3169.54.1.14
Parker, R., & Aggleton, P. (2003). HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Social Science & Medicine, 57(1), 13–24.
https://doi.org/10.1016/S0277-9536(02)00304-0
Richardson, F. C., & Manglos, N. D. (2013). Reciprocity and rivalry: A critical introduction to mimetic scapegoat theory. Pastoral Psychology, 62, 423–436.
https://doi.org/10.1007/s11089-012-0472-x
Rothschild, Z. K., Landau, M. J., Sullivan, D., & Keefer, L. A. (2012). A dual-motive model of scapegoating: Displacing blame to reduce guilt or increase control. Journal of Personality and Social Psychology, 102(6), 1148–1163.
https://doi.org/10.1037/a0027413
Rudman, L. A., & Ashmore, R. D. (2007). Discrimination and the Implicit Association Test. Group Process & Intergroup Relations, 10(3), 359–372.
https://doi.org/10.1177/1368430207078696
Schreger, C., & Kimble, M. (2017). Assessing civilian perceptions of combat veterans: An IAT study. Psychological Trauma: Theory, Research, Practice, and Policy, 9(1), 12–18.
https://doi.org/10.1037/tra0000191
Tam, T., Hewstone, M., Harwood, J., Voci, A., & Kenworthy, J. (2006). Intergroup contact and grandparent–grandchild communication: The effects of self-disclosure on implicit and explicit biases against older people. Group Process & Intergroup Relations, 9(3), 413–429.
https://doi.org/10.1177/1368430206064642
Van Brakel, W. H. (2006). Measuring health-related stigma—A literature review. Psychology, Health & Medicine, 11(3), 307–334.
https://doi.org/10.1080/13548500600595160
Vaughan, G., & Hogg, M. A. (2005). Introduction to social psychology (4th ed). Pearson Education Australia.
Yeh, M.-C., & Tung, H.-J. (2021). Stigma is associated with widening health inequities: Challenges from the current COVID-19 pandemic. American Journal of Public Health, 111(6), 1022–1023.
https://doi.org/10.2105/AJPH.2021.306265
Ajzen, I. (1993). Attitude theory and the attitude-behavior relation. In D. Krebs & P. Schmidt (Eds.), New directions in attitude measurement (pp. 41–57). Walter de Gruyter.
Allport, G. W. (1954). The historical background of modern social psychology. In G. Lindzay (Ed.), Handbook of social psychology (pp. 3–56). Addison Wesley.
Banaji, M. R., Baron, A. S., Dunham, Y., & Olson, K. (2007). The development of intergroup social cognition: Early emergence, implicit nature, and sensitivity to group status. In M. Killen & S. Levy (Eds.), Intergroup attitudes and relations in childhood through adulthood (pp. 87–102). Oxford University Press.
Bang, H. J., Noh, K. R., & Jung, S. J. (2010). The development of implicit and explicit race attitudes in Korean in the multi-cultural age [In Korean]. The Korean Journal of Developmental Psychology, 23(2), 125–140. https://bit.ly/3jtdLqU
Barrett, R., & Brown, P. J. (2008). Stigma in the time of influenza: Social and institutional responses to pandemic emergencies. The Journal of Infectious Diseases, 197(1), 34–37.
https://doi.org/10.1086/524986
Bonadonna, L. V., Saunders, M. J., Zegarra, R., Evans, C., Alegria-Flores, K., & Guio, H. (2017). Why wait? The social determinants underlying tuberculosis diagnostic delay. PLoS ONE, 12(9), Article e0185018.
https://doi.org/10.1371/journal.pone.0185018
Chang, S.-H., & Cataldo, J. K. (2014). A systematic review of global cultural variations in knowledge, attitudes and health responses to tuberculosis stigma. The International Journal of Tuberculosis and Lung Disease, 18(2), 168–173.
https://doi.org/10.5588/ijtld.13.0181
Charlesworth, T. E. S., & Banaji, M. R. (2019). Patterns of implicit and explicit attitude: I. Long-term change and stability from 2007 to 2016. Psychological Science, 30(2), 174–192.
https://doi.org/10.1177/0956797618813087
Des Jarlais, D. C., Galea, S., Tracy, M., Tross, S., & Vlahov, D. (2006). Stigmatization of newly emerging infectious diseases: AIDS and SARS. American Journal of Public Health, 96(3), 561–567.
https://doi.org/10.2105/AJPH.2004.054742
Furnham, A. (2003). Belief in a just world: Research progress over the past decade. Personality and Individual Differences, 34(5), 795–817.
https://doi.org/10.1016/S0191-8869(02)00072-7
Goffman, E. (1963). Stigma: Notes on the management of spoiled identity. Prentice Hall.
Greenwald, A. G., Banaji, M. R., Rudman, L. A., Farnham, S. D., Nosek, B. A., & Mellott, D. S. (2002). A unified theory of implicit attitudes, stereotypes, self-esteem, and self-concept. Psychological Review, 109(1), 3–25.
https://doi.org/10.1037/0033-295X.109.1.3
Greenwald, A. G., McGhee, D. E., & Schwartz, J. L. K. (1998). Measuring individual differences in implicit cognition: The Implicit Association Test. Journal of Personality and Social Psychology, 74(6), 1464–1480.
https://doi.org/10.1037//0022-3514.74.6.1464
Greenwald, A. G., Nosek, B. A., & Banaji, M. R. (2003). Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology, 85(2), 197–216.
https://doi.org/10.1037/0022-3514.85.2.197
Hatzenbuehler, M. L., Phelan, J. C., & Link, B. G. (2013). Stigma as a fundamental cause of population health inequalities. American Journal of Public Health, 103(5), 813–821.
https://doi.org/10.2105/AJPH.2012.301069
Heijnders, M., & Van Der Meij, S. (2006). The fight against stigma: An overview of stigma-reduction strategies and interventions. Psychology, Health & Medicine, 11(3), 353–363.
https://doi.org/10.1080/13548500600595327
Internet Trend. (2020, September 10). Logger [In Korean]. https://bit.ly/3amQ2mX
Jhangiani, R., & Tarry, H. (2014). Principles of social psychology (1st international ed.). https://bit.ly/3jx7xX7
John, T. (2021, June 1). The stigma of variant names. Cable News Network. https://cnn.it/3jxcqzr
Jordan, C. H., Logel, C., Spencer, S. J., & Zanna, M. P. (2012). Discrepancies between implicit and explicit attitudes, prejudices, and self-esteem: A model of simultaneous accessibility. In B. Gawronski & F. Strack (Eds.), Cognitive consistency: A fundamental principle in social cognition (pp. 202–222). Guilford Press.
Kang, E., Lee, S. Y., Kim, M. S., Jung, H., Kim, K. H., Kim, K.-N., … Sohn, J. H. (2021). The psychological burden of COVID-19 stigma: Evaluation of the mental health of isolated mild condition COVID-19 patients. Journal of Korean Medical Science, 36(3), Article e33.
https://doi.org/10.3346/jkms.2021.36.e33
Karpinski, A., & Steinman, R. B. (2006). The Single Category Implicit Association Test as a measure of implicit social cognition. Journal of Personality and Social Psychology, 91(1), 16–32.
https://doi.org/10.1037/0022-3514.91.1.16
Kim, S. H. (2002). Attitude and social distance towards minority groups in Korean society [In Korean]. Korean Journal of Social Issues, 1, 169–206. https://bit.ly/39DoRUo
Liu, R., Nicholas, S., Leng, A., Qian, D., Maitland, E., & Wang, J. (2021). The influencing factors of discrimination against recovered Coronavirus disease 2019 (COVID-19) patients in China: A national study. Human Vaccines & Immunotherapeutics. Advance online publication.
https://doi.org/10.1080/21645515.2021.1913966
Lohiniva, A.-L., Dub, T., Hagberg, L., & Nohynek, H. (2021). Learning about COVID-19-related stigma, quarantine and isolation experiences in Finland. PLoS ONE, 16(4), Article e0247962.
https://doi.org/10.1371/journal.pone.0247962
Nosek, B. A. (2007). Implicit–explicit relations. Current Directions in Psychological Science, 16(2), 65–69.
https://doi.org/10.1111/j.1467-8721.2007.00477.x
Nosek, B. A., & Smyth, F. L. (2007). A multitrait-multimethod validation of the Implicit Association Test. Experimental Psychology, 54(1), 14–29.
https://doi.org/10.1027/1618-3169.54.1.14
Parker, R., & Aggleton, P. (2003). HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Social Science & Medicine, 57(1), 13–24.
https://doi.org/10.1016/S0277-9536(02)00304-0
Richardson, F. C., & Manglos, N. D. (2013). Reciprocity and rivalry: A critical introduction to mimetic scapegoat theory. Pastoral Psychology, 62, 423–436.
https://doi.org/10.1007/s11089-012-0472-x
Rothschild, Z. K., Landau, M. J., Sullivan, D., & Keefer, L. A. (2012). A dual-motive model of scapegoating: Displacing blame to reduce guilt or increase control. Journal of Personality and Social Psychology, 102(6), 1148–1163.
https://doi.org/10.1037/a0027413
Rudman, L. A., & Ashmore, R. D. (2007). Discrimination and the Implicit Association Test. Group Process & Intergroup Relations, 10(3), 359–372.
https://doi.org/10.1177/1368430207078696
Schreger, C., & Kimble, M. (2017). Assessing civilian perceptions of combat veterans: An IAT study. Psychological Trauma: Theory, Research, Practice, and Policy, 9(1), 12–18.
https://doi.org/10.1037/tra0000191
Tam, T., Hewstone, M., Harwood, J., Voci, A., & Kenworthy, J. (2006). Intergroup contact and grandparent–grandchild communication: The effects of self-disclosure on implicit and explicit biases against older people. Group Process & Intergroup Relations, 9(3), 413–429.
https://doi.org/10.1177/1368430206064642
Van Brakel, W. H. (2006). Measuring health-related stigma—A literature review. Psychology, Health & Medicine, 11(3), 307–334.
https://doi.org/10.1080/13548500600595160
Vaughan, G., & Hogg, M. A. (2005). Introduction to social psychology (4th ed). Pearson Education Australia.
Yeh, M.-C., & Tung, H.-J. (2021). Stigma is associated with widening health inequities: Challenges from the current COVID-19 pandemic. American Journal of Public Health, 111(6), 1022–1023.
https://doi.org/10.2105/AJPH.2021.306265

Figure 1. Sample Stimulus Photographs
Note. The text in the sign in the photograph on the right says “Do not enter. Confirmed case of COVID-19 on this site.”
Table 1. Single-Category Implicit Association Test Steps to Measure Implicit Attitude Toward People With COVID-19
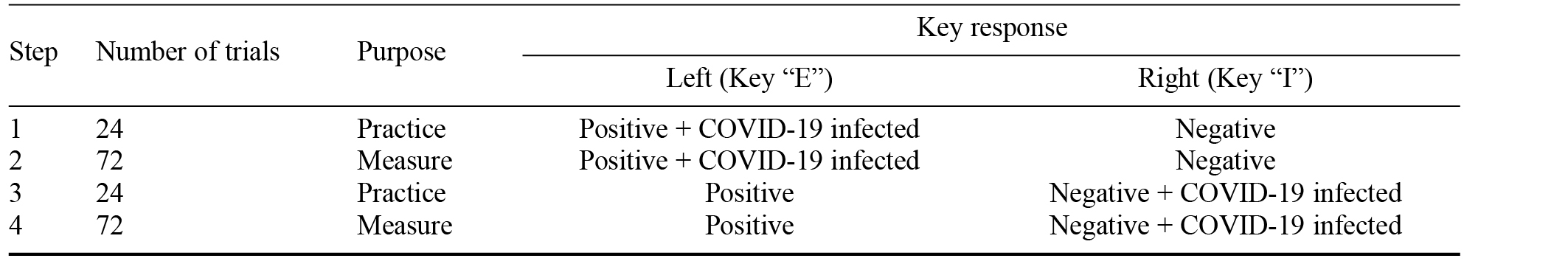
Table 2. Criteria for the Converted Adjusted Difference Values to Measure Implicit Attitude Toward People With COVID-19
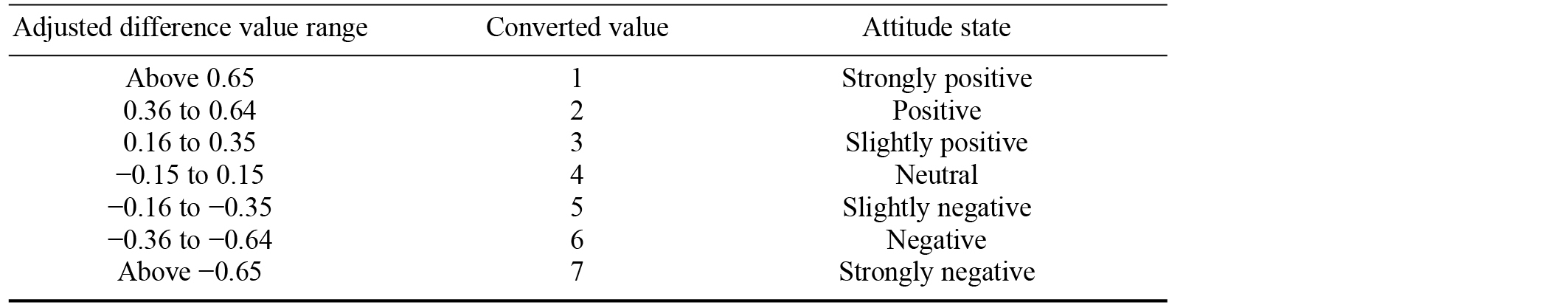
Note. A lower value indicates a positive attitude and a higher value indicates a negative attitude.
Table 3. Demographic Characteristics of the Participants
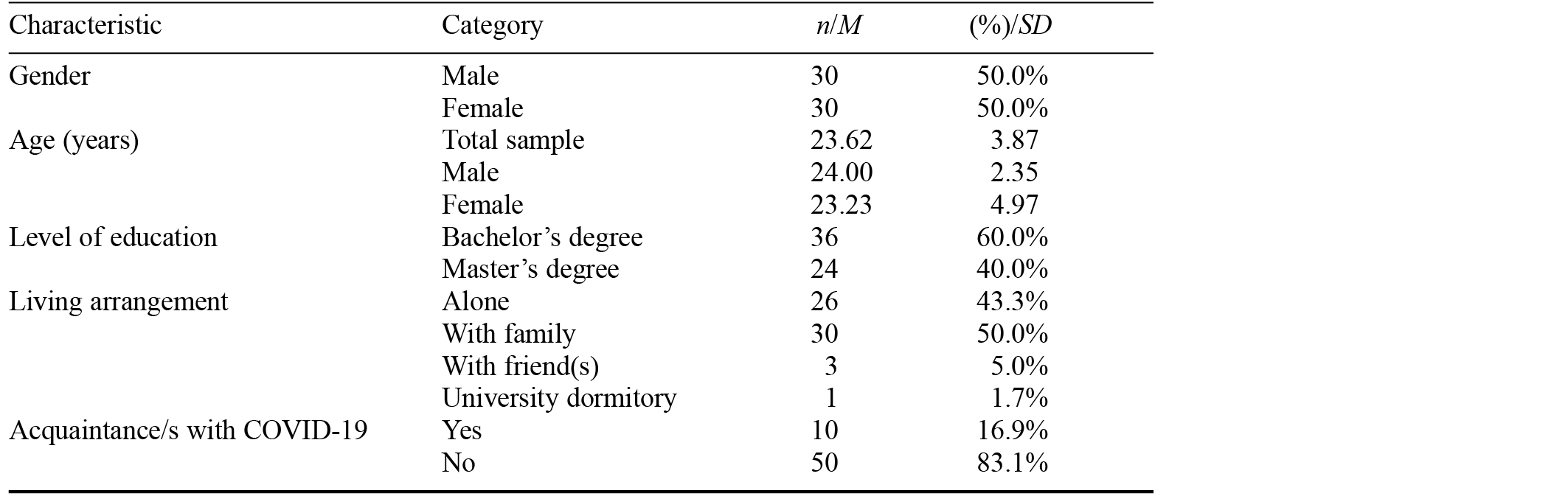
Note. N = 60.
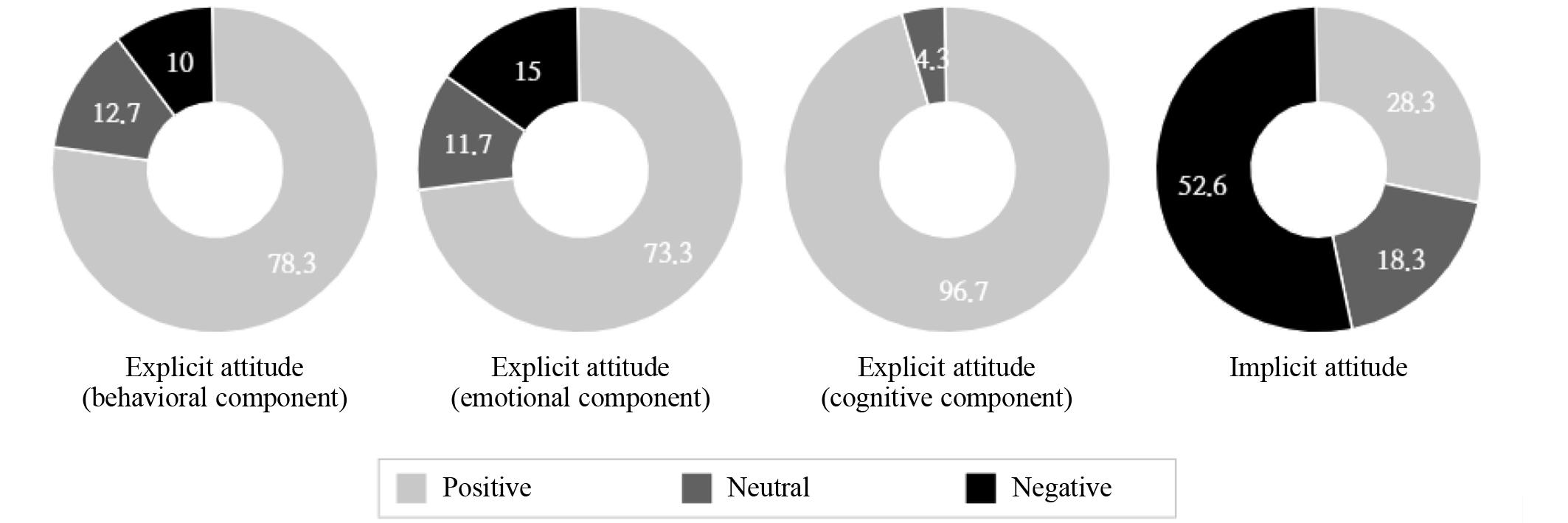
Figure 2. Percentage Comparison of Implicit and Explicit Attitudes Toward People With COVID-19
Note. N = 60. On the 7-point Likert scale, positive = score of 1–3 points for an item; neutral = score of 4 points; negative = score of 5–7 points.
Table 4. Correlation of Explicit and Implicit Attitudes Toward People With COVID-19
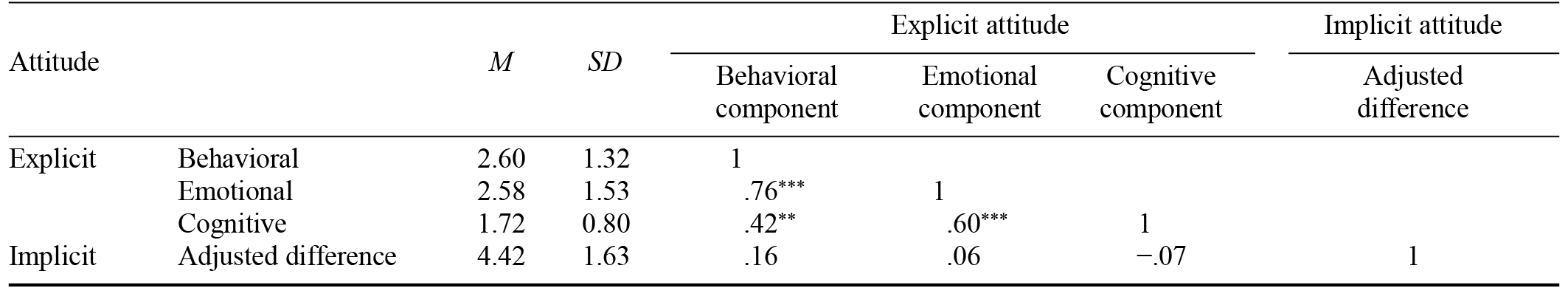
Note. * p < .05. ** p < .01. *** p < .001.
This research was supported by a grant from the National Research Foundation of Korea
funded by the government of the Republic of Korea (2020R1A2B5B01002082) and the Chung-Ang University Research Scholarship Grants in 2020.
Dong-Hee Cho, Red Cross College of Nursing, Chung-Ang University, 84 Heukseok-Ro, Dongjak-Gu, Seoul, 06974, Republic of Korea. Email: [email protected]